Data extracted in July 2024.
Planned article update: October 2025.
Highlights
Lung cancer accounted for 4.3% of all deaths in the EU and for around a fifth (19.8%) of all cancer-related deaths in the EU in 2021.
Among the 23 EU counties for which data are available, there were 520 700 hospital discharges of colorectal cancer in-patients in 2021
In 2021, at least 4.2% of all female deaths in Cyprus, Ireland and Luxembourg were from breast cancer; this was less than 2% in Bulgaria.
Among the EU countries, in 2021 male deaths from prostate cancer ranged from 1.4% in Bulgaria and Romania up to 4.5% in Denmark and Sweden.
Mammography units, 2022
This article presents an overview of European Union (EU) statistics related to a selection of the most common types of cancer: trachea, bronchus and lung cancer, hereafter referred to simply as lung cancer; colorectal cancer; breast cancer; and prostate cancer. For each of these 4 types of cancer, an analysis is provided that focuses on deaths from cancer and cancer healthcare (in terms of the average length of hospital stays for in-patients and the number of hospital discharges); there are also data on screenings. Accompanying articles on cancer statistics and on cancer screening provide an overview of statistics related to cancers in general and their prevention.
This article is 1 of a set of statistical articles concerning healthcare activities in the EU which forms part of an online publication on Health in the European Union – facts and figures.
Lung cancer
Within the EU, lung cancer accounted for around a fifth of all deaths from cancer
In 2021, nearly a quarter of a million (226 500) people died from lung cancer in the EU, almost a fifth (19.8%) of all deaths from cancer and 4.3% of the total number of deaths – see Table 1. The share of all deaths attributed to lung cancer was 5.5% among males, which was almost twice as high as the share (3.0%) recorded for females.
Among the EU countries, the share of the total number of deaths from lung cancer in 2021 peaked in Denmark and the Netherlands (both 6.0%), followed by Ireland (5.5%). By contrast, shares of less than 2.5% were recorded in Bulgaria (2.2%) and Lithuania (2.3%).
In 2021, the share of male deaths from lung cancer peaked in Greece (at 7.4%), while Spain and Malta both recorded shares of at least 7.0%. Sweden and Denmark were the only EU countries to report a higher share of female deaths than male deaths from lung cancer. Among females the highest share of female deaths from lung cancer was recorded in Denmark (6.1%). The Netherlands and Ireland were the only other EU countries with shares of more than 5.0%. Among the 25 EU countries where there was a higher share of male deaths than female deaths from lung cancer, the largest gender gap was reported in Greece, where the share of male deaths was 5.1% percentage points (pp) higher than for females. Spain, Malta and Cyprus also reported shares of male deaths from lung cancer that were more than 4 pp higher than the share for females. The smallest gender gap was reported in Ireland where the share of males deaths was only 0.2 pp higher than the share for females.
In 2021, the EU standardised death rate for lung cancer was 47.0 per 100 000 inhabitants, this was the highest among the cancerous causes of death, surpassing the rates for the other 3 types of cancer presented in this article. An analysis by sex and by age shows large differences in the standardised death rates for lung cancer: for males, the rate of 69.9 per 100 000 inhabitants, was almost 2.4 times as high as for females (29.5 per 100 000 inhabitants), although there are signs of this gender gap narrowing in recent years. As is typical for cancers as a whole, the standardised death rate for lung cancer for people aged 65 years and over (181.3 per 100 000 inhabitants aged 65 and over) was 12.5 times higher than for younger people (14.5 per 100 000 inhabitants aged less than 65 years).
Among the EU countries, by far the highest standardised death rate for lung cancer in 2021 was recorded in Hungary (77.9 per 100 000 inhabitants), followed by Croatia with a rate of 63.1 deaths per 100 000 inhabitants. Finland, Lithuania, Portugal and Sweden were the only EU countries to record standardised death rates for lung cancer that were below 40.0 per 100 000 inhabitants, with Sweden recording the lowest standardised death rate, at 32.5 deaths per 100 000 inhabitants.
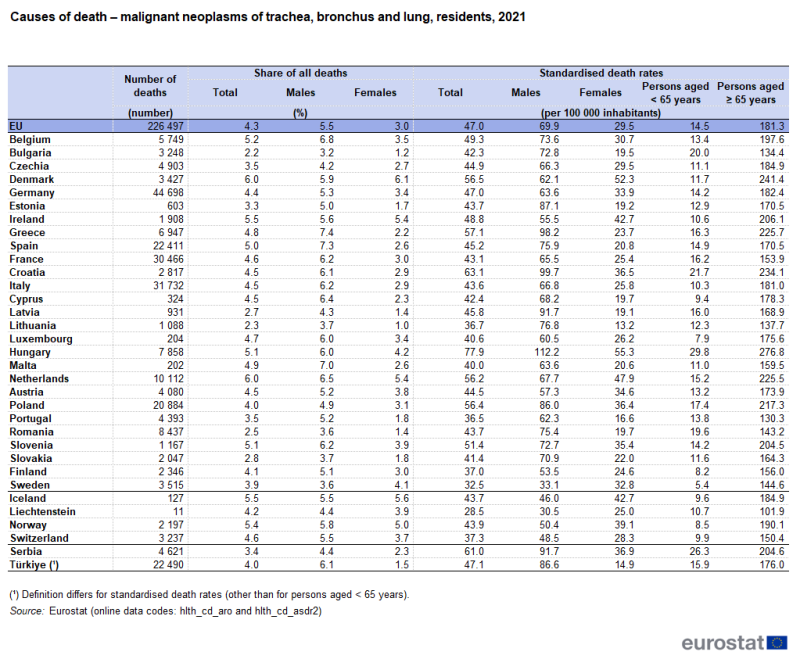
Source: Eurostat (hlth_cd_aro) and (hlth_cd_asdr2)
An analysis by sex reveals that, in 2021, the highest standardised death rate for lung cancer for both sexes was recorded in Hungary; with 112.2 deaths per 100 000 male inhabitants and 55.3 deaths per 100 000 female inhabitants. The lowest standardised death rate for lung cancer among males was recorded in Sweden, where the rate was 33.1 per 100 000 male inhabitants in 2021; this was considerably lower than in any of the other EU countries, as the next lowest death rate was 53.5 per 100 000 male inhabitants in neighbouring Finland. For females, the lowest standardised death rates for lung cancer were recorded in Lithuania (13.2 per 100 000 female inhabitants) and Portugal (16.6 per 100 000 female inhabitants).
More than 450 000 in-patient discharges for lung cancer, in 2021
Based on the data available for the EU countries, there were 458 700 discharges of lung cancer in-patients in 2021 (2020 data for Malta; no recent data for Denmark, Estonia, Greece or Luxembourg).
From Figure 1 it can be seen that the highest discharge rate for in-patients in 2021 was in Austria, where 234.1 in-patients per 100 000 inhabitants were discharged after diagnosis or treatment for lung cancer. This was closely followed by Germany, where the rate was 225.1 discharges per 100 000 inhabitants. Elsewhere, the rate ranged from 151.7 discharges per 100 000 inhabitants in Latvia to 31.8 discharges per 100 000 inhabitants in Malta (2020 data).
The average length of stay for lung cancer in-patients ranged from 3.5 days in Bulgaria to 14.7 days in Malta
Among the EU countries for which data are available (see Figure 1), in 2021 the average length of stay for lung cancer in-patients ranged from less than 5.0 days in Cyprus and Bulgaria, where the lowest average stay was recorded at 3.5 days, to 11.1 days in Ireland and Portugal and a peak of 14.7 days in Malta (2020 data). The average length of stay for lung cancer in-patients was typically longer than the average for all in-patients having been treated for neoplasms (whether malignant (cancer), in situ or benign).
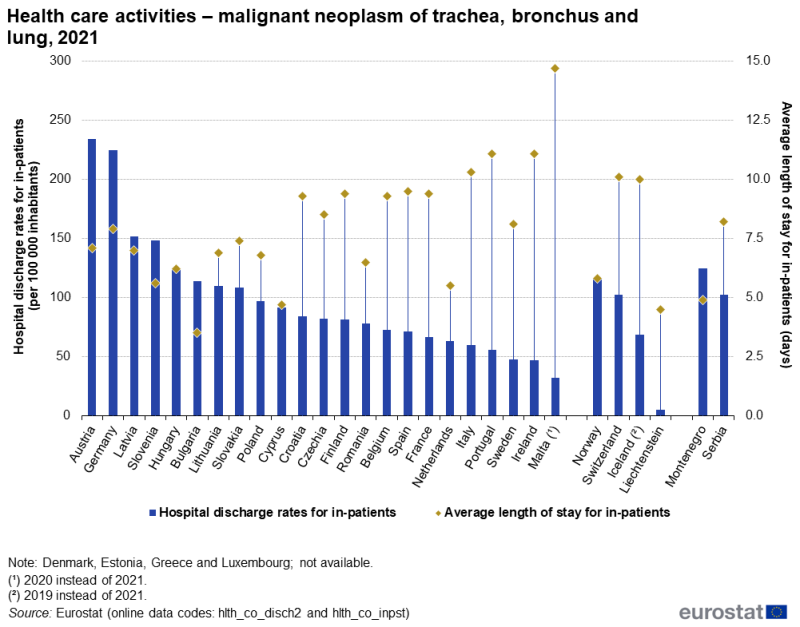
Source: Eurostat (hlth_co_disch2) and (hlth_co_inpst)
Colorectal cancer
Cyprus and Greece had the lowest share of deaths from colorectal cancer
In 2021, 132 300 people died from colorectal cancer in the EU, equivalent to 11.6% of all deaths from cancer and 2.5% of the total number of deaths from any cause – see Table 2. The share of deaths attributed to colorectal cancer was 2.8% for males and 2.2% for females, representing a much narrower gender gap compared with the one for lung cancer.
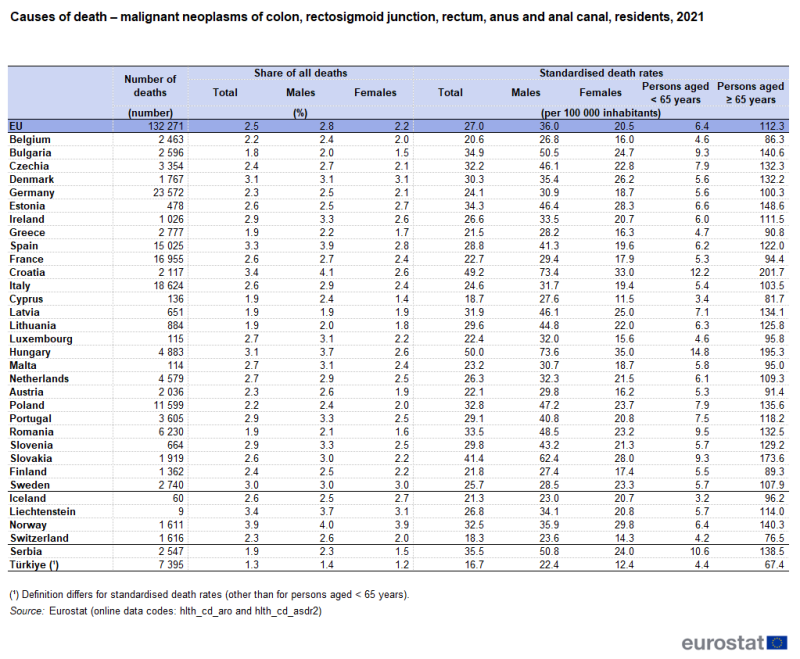
Source: Eurostat (hlth_cd_aro) and (hlth_cd_asdr2)
In 2021, the proportion of deaths attributed to colorectal cancer peaked among the EU countries in Croatia (3.4%), followed closely by Spain (3.3%). At the other end of the range, the lowest share of deaths from colorectal cancer was reported in Bulgaria (1.8%), with a slightly higher share recorded in Lithuania, Romania, Cyprus, Latvia and Greece (all 1.9%).
An analysis by sex reveals that Latvia recorded the lowest share of deaths attributed to colorectal cancer for males (1.9%), while Cyprus recorded the lowest share for females (1.4%). Croatia recorded the highest share of male deaths attributed to colorectal cancer in 2021, at 4.1%; Denmark recorded the highest share for females, with 3.1% of female deaths. Estonia and Sweden were the only EU countries, where the share of deaths attributed to colorectal cancer was higher among females than among males (0.3 and 0.09 pp respectively). The largest gender gap was reported in Croatia, where the share of male deaths from colorectal cancer was 1.5 pp higher than that for females, while the lowest gender gap was reported in Denmark and Latvia, both less than 0.1 pp.
In 2021, the EU standardised death rate for colorectal cancer was 27.0 per 100 000 inhabitants. An analysis by sex shows some differences in the standardised death rates for colorectal cancer: the EU rate was 1.8 times as high for males compared with females; this difference was nevertheless considerably lower than the corresponding ratio recorded for lung cancer.
As is typical for cancers as a whole, the standardised death rate for colorectal cancer for people aged 65 years and over was substantially higher than it was for younger people. When expressed as a ratio, the EU’s standardised death rate for people aged 65 years and over was 18 times as high as it was for younger people, a higher ratio than for lung cancer (12 times as high) and also higher than the ratio for all cancers (14 times as high).
As with lung cancer, the highest standardised death rate for colorectal cancer among the EU countries in 2021 was recorded in Hungary (50.0 per 100 000 inhabitants), followed by Croatia (49.2 per 100 000 inhabitants) and Slovakia (41.4 per 100 000 inhabitants). Cyprus was the only EU country to record a standardised death rate for colorectal cancer that was below 20.0 per 100 000 inhabitants.
In 2021, Hungary and Croatia recorded the highest standardised death rates for colorectal cancer for both males and females (73.6 and 35.0 deaths per 100 000 males/females, respectively). Belgium recorded the lowest standardised death rate for males (26.8) and Cyprus the lowest rate for females (11.5). In all EU countries, standardised death rates for colorectal cancer were higher among males than among females. The narrowest gender gap was recorded in Sweden (where the rate for males was 5.2 deaths per 100 000 inhabitants higher than that for females); Denmark also recorded a difference between the sexes that was less than 10.0 deaths per 100 000 inhabitants. By contrast, in Croatia, Hungary and Slovakia, the rates for males were 34.4 to 40.4 deaths per 100 000 inhabitants higher than those for females.
Croatia reported the highest in-patient discharge rates for colorectal cancer
Based on available data for the EU countries, there were 520 700 hospital discharges of colorectal cancer in-patients in 2021 (2020 data for Malta; no recent data for Denmark, Estonia, Greece or Luxembourg).
Figure 2 shows that the highest discharge rate for colorectal cancer in-patients in 2021 was recorded in Croatia (316.7 in-patient discharges per 100 000 inhabitants), followed at some distance by Bulgaria, Austria and Latvia (where there were 258.1, 239.3 and 238.7 in-patient discharges per 100 000 inhabitants, respectively). None of the remaining EU countries for which data are available reported a rate in excess of 200 discharges per 100 000 inhabitants. The lowest rates were reported for Ireland and Malta (2020 data), at 54.5 and 40.9 discharges per 100 000 inhabitants, respectively.

Source: Eurostat (hlth_co_disch2) and (hlth_co_inpst)
In 2021, among the 23 EU countries for which data are available (see Figure 2), the average length of stay for colorectal cancer in-patients ranged from 4.8 days in Bulgaria to 14.0 days in Malta (2020 data).
Breast cancer
In Cyprus, Ireland and Luxembourg, more than 4.0% of all deaths among females were from breast cancer
In 2021, 84 800 people died from breast cancer in the EU, of which just under 1 000 were males and the vast majority (83 900) were females. As such, deaths from breast cancer made up 7.4% of all deaths from cancer; among females, breast cancer accounted for 16.5% of all deaths from cancer.
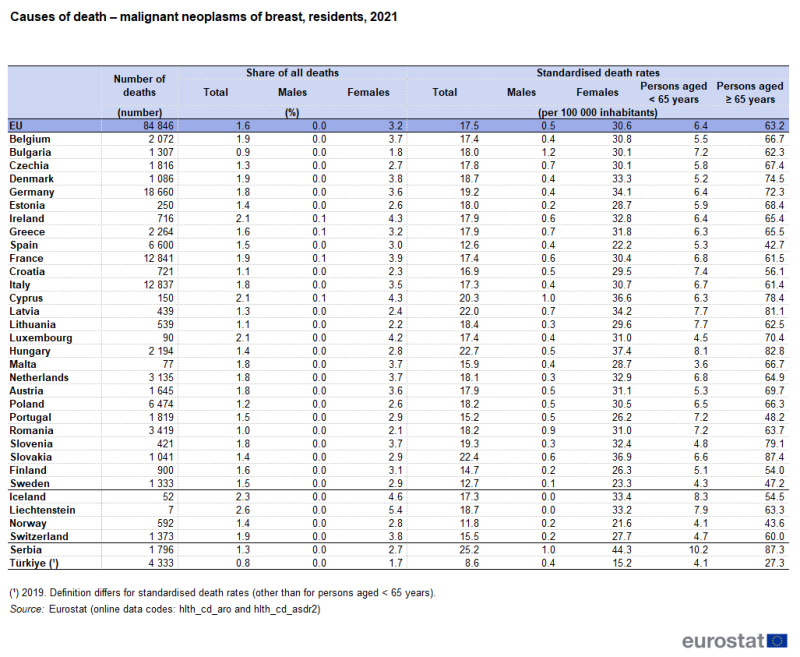
Source: Eurostat (hlth_cd_aro) and (hlth_cd_asdr2)
In 2021, breast cancer was the underlying cause of death for 1.6% of the total number of deaths in the EU (see Table 3); among females, breast cancer accounted for 3.2% of all deaths. Across the EU countries, the share of deaths from breast cancer among females in 2021 was highest at 4.3% in Cyprus and Ireland, followed closely by a 4.2% share in Luxembourg. By contrast, the lowest share was 1.8% in Bulgaria.
The EU standardised death rate for breast cancer was 30.6 per 100 000 inhabitants in 2021 for females and 0.5 per 100 000 inhabitants for males. As is typical for cancers as a whole, the standardised death rate for breast cancer for people aged 65 years and over (63.2 per 100 000 inhabitants) was much higher than it was for younger people aged less than 65 (6.4 per 100 000 inhabitants). Nevertheless, this age difference was somewhat narrower than for all malignant neoplasms in general: the standardised death rate for breast cancer among people aged 65 years and over was 10 times as high as it was for younger people, compared with 14 times as high for all cancers.
In 2021, the highest standardised death rate for breast cancer among females was recorded in Hungary (37.4 deaths per 100 000 female inhabitants), followed by Slovakia (36.9 per 100 000 female inhabitants) and Cyprus (36.6 per 100 000 female inhabitants). Standardised death rates for breast cancer for females were below 30.0 per 100 000 in 8 EU countries: Lithuania, Croatia, Estonia, Malta, Finland, Portugal, Sweden and Spain; the last of these had the lowest rate, at 22.2 per 100 000 female inhabitants. Among males, the standardised death rate for breast cancer ranged from 0.1 in Sweden to 1.2 per 100 000 male inhabitants in Bulgaria.
In 18 of the 27 EU countries, the standardised death rate for females for breast cancer in 2021 was higher than that for lung cancer; the gap was particularly large in Cyprus, Lithuania, Latvia and Slovakia. The most notable exceptions – where there were, among females, 15 to 19 more deaths per 100 000 female inhabitants from lung cancer than from breast cancer – were Denmark, Hungary and the Netherlands.
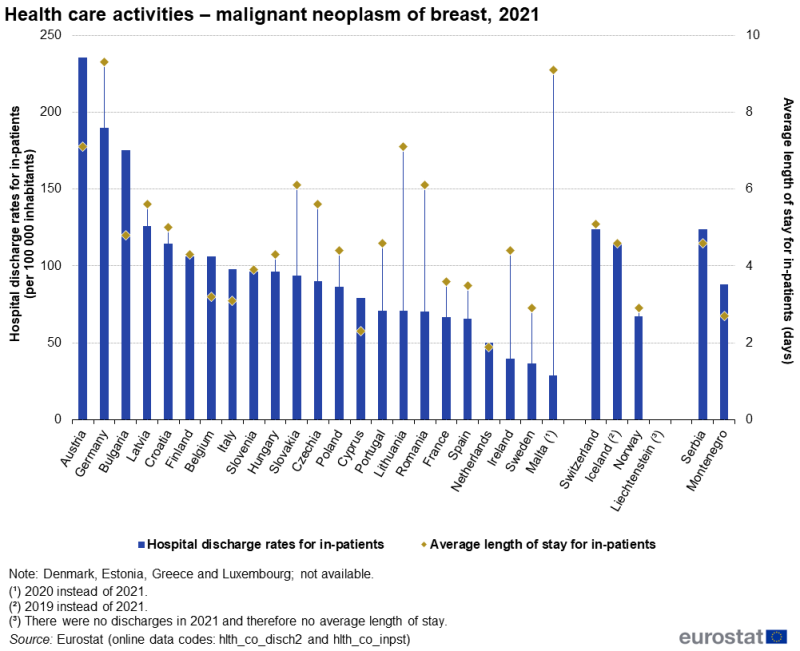
Austria recorded the highest in-patient discharge rates for breast cancer
Based on available data for the EU countries, there were 447 100 discharges of breast cancer in-patients in 2021 (2020 data for Malta; no recent data for Denmark, Estonia, Greece or Luxembourg).
Figure 3 shows that the highest discharge rate for in-patients in 2021 was recorded in Austria, the only EU country to report more than 200 in-patients per 100 000 inhabitants were discharged after diagnosis or treatment for breast cancer. In a majority of the EU countries for which data are available (16 out of 23; see Figure 3), the in-patient discharge rate for breast cancer was below 100 discharges per 100 000 inhabitants. Malta (2020 data), Sweden and Ireland recorded the lowest rates, with fewer than 40.0 discharges per 100 000 inhabitants.
Source: Eurostat (hlth_co_disch2) and (hlth_co_inpst)
The average length of stay for breast cancer in-patients was longest in Germany and Malta
In 2021, the average length of stay for breast cancer in-patients among the majority of the 23 EU countries for which data are available (see Figure 3) ranged from 2.9 days in Sweden to 7.1 days in Austria and Lithuania. The Netherlands and Cyprus were below this range (1.9 and 2.3 days, respectively), while Malta (9.1 days; 2020 data) and Germany (9.3 days) were above it. A comparison with the average length of stay for all in-patients having been treated for neoplasms shows that in nearly all EU countries the average length of stay for breast cancer in-patients was shorter.
Breast cancer screening rates were 80% or higher in the Nordic EU countries
The information presented for breast cancer screening is administrative data from screening programmes. The standard analysis is the proportion of women aged 50 to 69 years who had received a mammography within the previous 2 years; in practice, some countries use different age ranges or screening frequencies (see Figure 4 for details on specific age ranges).
Data on breast cancer screening rates for women are available for 2022 (2021 data for Denmark and Hungary) for 25 of the EU countries; see Figure 4 for more details. Among these, screening rates were below 40.0% in 5 EU countries, with the lowest rate of 28.5% reported in Slovakia (women aged 40–69 years). At the other end of the range, Denmark (83.0%; 2021 data), Finland (81.6%) and Sweden (81.0%; women aged 40–74 years) reported screening rates that were above four fifths; Slovenia had the next highest rate, at 78.3%.
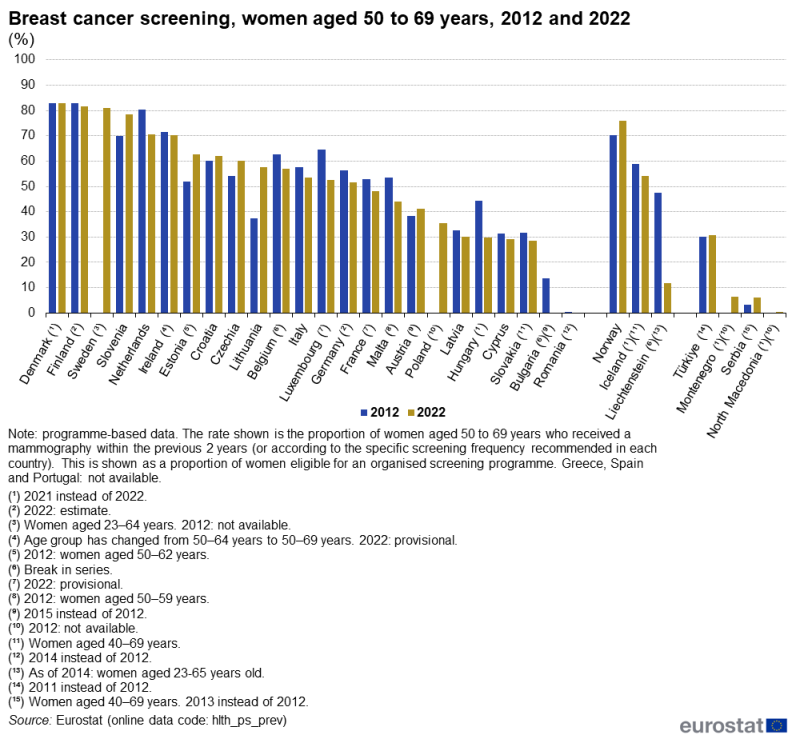
(%)
Source: Eurostat (hlth_ps_prev)
A comparison of data for the 2 years shown in Figure 4 indicates that breast cancer screening rates increased in 6 of the 22 EU countries for which data are available, with the largest increase (in percentage point terms) observed in Lithuania (up 20.1 points). There was no change in the rate for Denmark, which had the highest screening rate. In the 13 EU countries where screening rates fell between the 2 years shown, the decreases were generally relatively small. Nevertheless, falls in excess of 9.0 percentage points were observed in Hungary (2012–21), Luxembourg, the Netherlands and Malta (note that the age range changed over time).
Figure 5 indicates the availability of equipment solely intended for conducting mammographies. Relative to the size of population, this type of equipment was most widely available in 2022 in Greece (7.3 units per 100 000 inhabitants) and Cyprus (6.1 units per 100 000 inhabitants). The number of mammography units was also relatively high – within the range of 3.1 to 3.7 units per 100 000 inhabitants – in Italy, Belgium (2020 data), Finland, Bulgaria and Croatia. By contrast, there were fewer than 1.0 mammography units per 100 000 inhabitants in France and Germany (both hospitals only).
The largest increases between 2012 and 2022 in the availability of mammography units relative to the size of population were recorded in Greece and Cyprus, up 1.8 and 1.5 units per 100 000 inhabitants, respectively. By contrast, the availability of these units fell in 10 of the 24 EU countries for which data are available (see Figure 5), with the largest decrease registered in Malta (note that there is a break in series).

(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_medim)
Comparing the data presented in Figures 4 and 5 – and leaving aside Germany and France where there is only partial coverage of the availability of mammography units – breast cancer screening rates in Sweden, Czechia, Slovenia, Estonia, Denmark and Luxembourg appeared to be relatively high compared with the availability of mammography units, implying a higher average intensity of use or a greater use for screening of units other than ones solely for mammographies. By contrast, a relatively low screening rate was observed in Cyprus combined with a relatively high availability of mammography units.
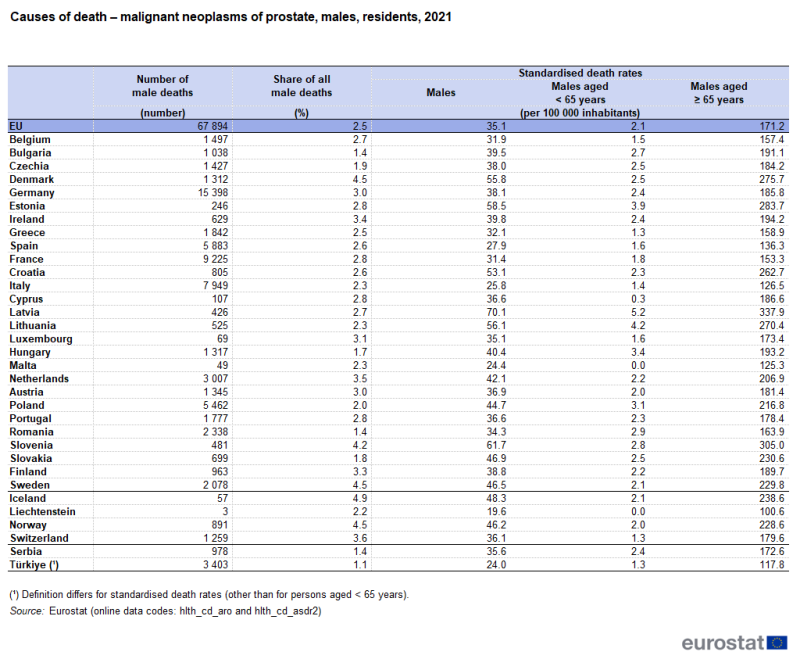
Prostate cancer
In Sweden, the standardised death rate for prostate cancer for males was higher than the equivalent rate for lung cancer
In 2021, 67 900 males died from prostate cancer in the EU (see Table 4), equivalent to 10.7% of all male deaths from cancer and 2.5% of the total number of male deaths from any cause.
Source: Eurostat (hlth_cd_aro) and (hlth_cd_asdr2)
Among the EU countries, the share of deaths among males that were attributed to prostate cancer was as low as 1.4% in Bulgaria and Romania, and as high as 4.5% in Denmark and Sweden.
In 2021, the EU standardised death rate for prostate cancer was 35.1 per 100 000 male inhabitants, slightly lower than the equivalent rate for colorectal cancer (36.0 per 100 000 male inhabitants). As is common for cancers, the standardised death rate for prostate cancer for men aged 65 years and over was many times higher than it was for younger males. Nevertheless, the gap between these rates was particularly wide for prostate cancer: when expressed as a ratio, the rate for men aged 65 years and over was 81 times as high as it was for younger males (aged less than 65 years).
Some of the highest standardised death rates for prostate cancer in 2021 were recorded across the northern EU countries, with rates above 45.0 per 100 000 male inhabitants recorded for all 3 Baltic countries and 2 of the 3 Nordic EU countries (Denmark and Sweden); rates above this level were also recorded in Slovenia, Croatia and Slovakia. There were 3 southern EU countries – Spain, Italy and Malta – that reported death rates for prostate cancer below 30.0 per 100 000 male inhabitants, the lowest rate was in Malta (24.4 per 100 000 male inhabitants).
As noted above, the standardised death rate in 2021 for prostate cancer in the EU was slightly lower than the equivalent rate for males for colorectal cancer. However, this was the case in a minority (11) of EU countries: in fact, it was higher in the remaining 16 EU countries. Sweden was the only EU country where the standardised death rate for males for prostate cancer was higher than the equivalent rate for males for lung cancer.
Germany and Austria reported the highest in-patient discharge rates for prostate cancer
Based on available data for the EU countries in 2021 (2020 data for Malta; no recent data for Denmark, Estonia, Greece or Luxembourg), there were 260 900 discharges of prostate cancer in-patients.
The highest in-patient discharge rates for prostate cancer in 2021 were recorded in Germany (where 270 in-patients per 100 000 male inhabitants were discharged) and Austria (248 in-patients per 100 000 male inhabitants were discharged); see Figure 6. In 14 of the EU countries for which recent data are available, the discharge rate for prostate cancer was below 100 discharges per 100 000 male inhabitants, dropping to less than 50 discharges per 100 000 male inhabitants in Romania, Ireland and Malta (where the lowest rate was recorded, at 13.9 discharges per 100 000 male inhabitants; 2020 data).

Source: Eurostat (hlth_co_disch2) and (hlth_co_inpst)
Compared with the average for all neoplasms, the average length of stay for prostate cancer in-patients was particularly long in Malta
In 2021, among the EU countries for which data are available (see Figure 6 for more details concerning data availability), the average length of stay for male prostate cancer in-patients generally ranged from 4.4 days to 9.9 days; Malta (18.9 days; 2020 data) was above this range and Cyprus (3.7 days), Sweden (3.6 days) and the Netherlands (2.4 days) were below it.
Source data for tables and graphs
Key concepts
Data sources
An in-patient is a patient who is formally admitted (or ‘hospitalised’) to an institution for treatment and/or care and stays for a minimum of 1 night or more than 24 hours in the hospital or other institution providing in-patient care. An in-patient or day care patient is discharged from hospital when formally released after a procedure or course of treatment (episode of care). A discharge may occur because of the finalisation of treatment, signing out against medical advice, transfer to another healthcare institution, or because of death.
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised death rate (rather than crude) can be compiled which is independent of the age and sex structure of a population: this is done as most causes of death vary significantly by age and according to sex and the standardisation facilitates comparisons of rates over time and between countries.
Statistics on causes of death provide information on mortality patterns, supplying information on developments over time in the underlying causes of death. This source is documented in more detail in this article on Causes of death statistics - methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Causes of death are classified according to the 86 causes in the European shortlist, which is based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10). Chapter II of the ICD covers neoplasms, the following ICD-10 codes were described in this article:
- C18 to C21 malignant neoplasm of colon, rectosigmoid junction, rectum, anus and anal canal
- C33 to C34 malignant neoplasm of trachea, bronchus and lung
- C50 malignant neoplasm of breast
- C61 malignant neoplasm of prostate
The causes of death statistics manual provides an overview of the definitions, classifications and variables, both for mandatory variables and variables provided on a voluntary basis.
Statistics on healthcare resources (such as personnel and medical equipment) and healthcare activities (such as information on surgical operations, procedures and hospital discharges) are documented in this article on Healthcare non-expenditure statistics - methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For hospital discharges and the length of stay in hospitals, the International Shortlist for Hospital Morbidity Tabulation (ISHMT) is used to classify data from 2000 onwards; Chapter II covers neoplasms and includes the following headings (among others):
- malignant neoplasm of colon, rectum and anus (0201)
- malignant neoplasms of trachea, bronchus and lung (0202)
- malignant neoplasm of breast (0204)
- malignant neoplasm of prostate (0207)
For country specific notes, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
The Healthcare non-expenditure statistics manual provides an overview of the classifications, both for mandatory variables and variables provided on a voluntary basis.
Data on screening based on National Programmes
The data on screening for breast cancer (referring to the population aged 50 to 69 years) used in this article come from programme-based data. Breast cancer screening rates show the proportion of women (eligible for screening) that have been screened. This is based on the number of women aged 50 to 69 years who had received a bilateral mammography within the 2 years prior to the reference date (or according to the specific screening frequency recommended in each country) as a share of all women eligible for an organised screening programme.
For country specific notes on these data collections, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
Tables in this article use the following notation
| Value in italics | estimate or provisional data |
| Value is : | not available |
<context>
Context
The most frequently occurring forms of cancer in the EU are lung, colorectal, breast, pancreas and prostate cancers. Among males, lung cancer is the most frequent cause of death from cancer; the standardised death rate in the EU in 2021 for lung cancer was approximately double that for colorectal cancer and prostate cancer. Among females, breast cancer and lung cancer are the most common causes of death from cancer.
Primary prevention offers the most cost-effective, long-term strategy for reducing the burden of diseases in the EU; it involves tackling major health determinants, such as smoking, unhealthy diets and physical inactivity. The European Commission has supported many projects related to health determinants and health promotion in general.
Secondary prevention aims to reduce mortality by early detection of cancer through screening. In December 2003, a Council Recommendation on cancer screening was adopted, setting out principles of best practice in the early detection of cancer. A proposal to update the 2003 Recommendation to reflect the latest available scientific advice was adopted by the European Council on 9 December 2022. Council Recommendation (2022/C 473/01) is a key element of the EU’s Cancer Screening Scheme. The scheme is 1 of the flagship initiatives of Europe’s Beating Cancer Plan, a key pillar of a stronger European Health Union.
Europe’s Beating Cancer Plan supports EU countries’ work to prevent cancer and to ensure a high quality of life for cancer patients, survivors, their families and carers. It is structured around a number of key areas where the EU can add most value:
- prevention,
- early detection,
- diagnosis and treatment,
- quality of life of cancer patients and survivors.
</context>
Explore further
Other articles
Online publications
Health status – selected diseases and related health problems
Causes of death
Healthcare activities
- Cancer screening statistics
- Hospital discharges and length of stay
- Surgical operations and procedures
Methodology
General health statistics articles
Database
- Health (hlth), see
- Health care (hlth_care)
- Health care resources (hlth_res)
- Health care facilities (hlth_facil)
- Health care activities (hlth_act)
- Hospital discharges - national data (hlth_hosd)
- Length of stay in hospital (hlth_hostay)
- Operations, procedures and treatment (hlth_oper)
- Preventive services (hlth_prev)
- Preventive cancer screenings - programme data (hlth_ps_prev)
- Health care resources (hlth_res)
- Causes of death (hlth_cdeath)
- General mortality (hlth_cd_gmor)
- Causes of death - deaths by country of residence and occurrence (hlth_cd_aro)
- Causes of death - standardised death rate by NUTS 2 region of residence (hlth_cd_asdr2)
- General mortality (hlth_cd_gmor)
Thematic section
Publications
Selected datasets
Methodology
Manuals and guidelines
Metadata
- Causes of death (SIMS metadata file – hlth_cdeath_sims)
- Health care resources (ESMS metadata file – hlth_res_esms)
