Archive:Healthcare provision statistics
- Data extracted in April 2015. Most recent data: Further Eurostat information, Main tables and Database. Planned article update: April 2016.
This article presents key statistics on non-monetary aspects of healthcare in the European Union (EU); these data complement the data on healthcare expenditure. An individual’s state of health and that of the population in general is influenced by genetic and environmental factors, cultural and socioeconomic conditions, as well as the healthcare services that are available to prevent and to treat illness and disease.
Non-monetary statistics may be used to evaluate how a country’s healthcare system responds to the challenge of universal access to good healthcare, through measuring human and technical resources, the allocation of these resources and the demand by patients. This article presents statistics on healthcare professionals, hospital beds and hospital discharges of in-patients and day care patients.

(thousands)
Source: Eurostat (hlth_rs_prs1)
Source: Eurostat (hlth_rs_prs1), (hlth_rs_spec) and (demo_pjan)

(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_phys) and (demo_pjan)
Source: Eurostat (hlth_rs_prs1) and (demo_pjan)
(per 100 000 inhabitants)
Source: Eurostat (tps00046), (hlth_rs_bds) and (demo_pjan)

(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)
(ISHMT — international shortlist for hospital morbidity tabulation), 2012
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)

(ISHMT — international shortlist for hospital morbidity tabulation), 2012
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch4)

(days)
Source: Eurostat (hlth_co_inpst)

(ISHMT — international shortlist for hospital morbidity tabulation), average length of stay, 2012
(days)
Source: Eurostat (hlth_co_inpst)
Main statistical findings
Healthcare personnel: physicians
There were approximately 1.7 million physicians working in the EU
In 2012, there were approximately 1.7 million physicians in the EU-28 (see Figure 1), an increase of 227 thousand compared with 10 years earlier.
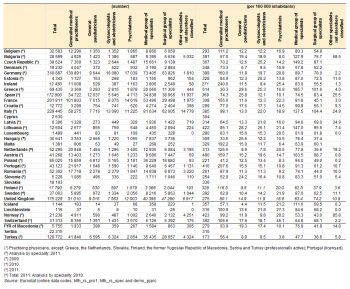
In the context of comparing healthcare services across EU Member States, Eurostat uses the concept of practising physicians, although for some Member States (see Table 1 for more details) data are only available for professionally active or licensed physicians.
Greece had the highest number of physicians per 100 000 inhabitants
One of the key indicators for measuring healthcare personnel is the total number of physicians, expressed per 100 000 inhabitants. Greece recorded the highest ratio among the EU Member States, at 614 per 100 000 inhabitants (2011 data for professionally active physicians). Austria (490), Lithuania (422) and Portugal (410; physicians licensed to practise) had the next highest ratios and were the only other Member States to record in excess of 400 physicians per 100 000 inhabitants. In contrast, there were fewer than 270 physicians per 100 000 inhabitants in Romania, Slovenia and Poland, where the lowest ratio was recorded (221 physicians per 100 000 inhabitants).
Spain was the only EU Member State to report having more surgical specialists than general medical practitioners or medical specialists
Table 1 provides statistics on physicians by seven specialities or groups of specailities: the three most common across the EU Member States (see Table 1 for data availability; no data available for Cyprus or Slovakia) were the groups of generalist medical practitioners, medical specialists and surgical specialists. In 13 of the Member States, including Germany, France and the United Kingdom, generalist medical practitioners were more common than any of the other specialities or groups of specialists shown in the table. In contrast, there were more medical specialists in 12 of the Member States (including Italy), leaving Spain as the only Member State to record a higher number of surgical specialists.
In 2012, the highest ratios of generalist medical practitioners to population size — in excess of 200 per 100 000 inhabitants — were recorded in Ireland and Portugal (2011 data). The highest ratios for medical specialists were found in Greece (186 per 100 000 inhabitants; 2011 data), the Czech Republic (149; 2011 data) and Lithuania (147; 2011 data), while the highest ratios for surgical specialists were recorded in Italy (104 per 100 000 inhabitants; 2011 data) and Greece (102; 2011 data).
Figure 2 presents information on the gender distribution of the number of physicians. In 2012, the highest share of male physicians was recorded in Luxembourg, where in excess of two thirds (68.9 %) of all physicians were men. Men also accounted for a relatively high share — more than 6 out of 10 — of the physicians in Belgium (2011 data), Malta, Italy (2011 data) and Greece (2011 data). By contrast, all three of the Baltic States, as well as Romania, Croatia and Slovenia (all 2011 data) were characterised by a high proportion of female physicians, the share of women rising to 74.1 % in Estonia and 74.3 % in Latvia.
Healthcare personnel: nursing and caring professionals
Nursing professionals (ISCO 08 code 2221) assume responsibility for the planning and management of patient care, including the supervision of other healthcare workers, working autonomously or in teams with medical doctors and others in the application of preventive and curative care. In 2012, there were 3.1 million practising nursing professionals in the 25 EU Member States for which data are available (see Table 2 for more information concerning the data coverage for individual Member States).
Ireland had the highest number of nursing professionals relative to population size
Ireland had more than 1 250 professionally active nursing professionals per 100 000 inhabitants in 2012, which was the highest ratio among the EU Member States; Luxembourg and Sweden (2011 data) also recorded in excess of 1 000 practising nursing professionals per 100 000 inhabitants. The number of nursing professionals was otherwise generally within the range of 430–1 000 per 100 000 inhabitants in most of the remaining Member States, with Slovenia (221), Greece (179; 2009 data), Croatia (103), Finland (94; 2011 data) and Romania (44) recording lower ratios.
As with professional nurses, midwifery professionals (ISCO 08 code 2222) plan, manage, provide and evaluate care services. Midwives do so before, during and after pregnancy and childbirth, providing delivery care for reducing health risks to women and new-born children; they may work autonomously or in teams with other healthcare providers.
There were almost 165 thousand midwives in the EU
In 2012, there were almost 165 thousand practising midwives in the EU (no data for Cyprus; see Table 2 for more information concerning the data coverage for individual EU Member States).
In 2012, Sweden and Poland had the highest ratios of midwives relative to their populations, at 74 per 100 000 inhabitants (2011 data) and 63 per 100 000 inhabitants respectively. At the other end of the range, by far the lowest ratio was recorded in Slovenia, where there were, on average, just 6 midwives per 100 000 inhabitants.
Nursing associate professionals (ISCO 08 code 3221) provide basic nursing and personal care to people suffering from the effects of ageing, illness, injury, or other physical or mental impairment; they may also provide health advice to patients and families, or monitor patients’ conditions. Nursing associate professionals generally work under the supervision of, and in support of implementation of health care, treatment and referrals plans established by medical, nursing and other health professionals.
There were almost 580 thousand nursing associate professionals in the EU
Health care is organised in different ways across the EU Member States and this is reflected in the data for nursing associate professionals insofar as some countries do not recognise this type of professional. Subject to data availability (see Table 2 for more information concerning the data coverage for individual Member States), there were 13 Member States where there were no nursing associate professionals. Relative to population size, there were 951 nursing associate professionals in Finland for every 100 000 inhabitants (2011 data). This was considerably higher than in any of the other EU Member States, as the next highest ratio was recorded in Slovenia (595 nursing associate professionals per 100 000 inhabitants), while Denmark (2009 data) and Romania also recorded ratios of more than 500 nursing associate professionals per 100 000 inhabitants.
Health care assistants, or caring professionals, include all health care assistants irrespective of where they work, be they assistants in institutions (ISCO 08 code 5321), home-based personal care workers (ISCO 08 code 5322) or personal care workers not elsewhere classified (ISCO 08 code 5329).
More than 2.1 million people worked as health care assistants in the EU
Based on the data available in Table 2 (note there are no data for Germany or the United Kingdom) there were more than 2.1 million health care assistants working in the EU.
The number of health care assistants per 100 000 inhabitants in Finland and the Netherlands was considerably higher than in the other EU Member States
Finland had more than 1 900 practising health care assistants per 100 000 inhabitants in 2010, which was the highest ratio among the EU Member States, while the Netherlands had a ratio of just under 1 900 per 100 000 inhabitants (2011 data); Denmark (2009 data), Spain and Italy were the only other Member States to record at least 800 practising health care assistants per 100 000 inhabitants.
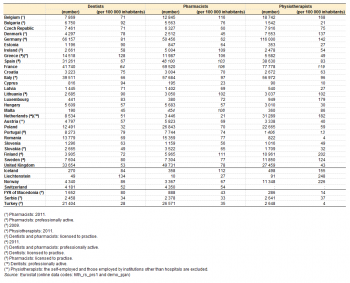
Healthcare personnel: dentists, pharmacists and physiotherapists
Table 3 provides an overview for 2012 of the number of dentists, pharmacists and physiotherapists practising in the EU Member States. There were over 330 thousand dentists in the EU-28, over 410 thousand pharmacists and over 450 thousand physiotherapists (see Table 3 for information concerning differences in data coverage for individual Member States).
Greece had the highest number of dentists per 100 000 inhabitants
Dentists (ISCO 08 code 2261) diagnose, treat and prevent diseases, injuries and abnormalities of the teeth, mouth, jaws and associated tissues. On the basis of a comparison in relation to population numbers, Greece recorded the highest number of dentists, at 128 per 100 000 inhabitants (2011 data for professionally active dentists). This was considerably higher than in any of the other EU Member States, as Cyprus (94), Bulgaria (92), Estonia and Lithuania (both 90) had the next highest ratios. By contrast, there were fewer than 50 dentists per 100 000 inhabitants in Slovakia (49; professionally active dentists), Malta (45) and Poland (32).
Belgium, France and Finland had the highest number of pharmacists per 100 000 inhabitants
Pharmacists (ISCO 08 code 2262) store, preserve, compound, dispense and sell medicinal products (irrespective of location) and may also provide advice on the proper use and adverse effects of drugs and medicines following prescriptions issued by medical doctors and other health professionals.
Taking into account the size of each country in population terms, Belgium recorded the highest number of pharmacists per 100 000 inhabitants, at 116 in 2011. Access to pharmacists was also relatively high in Finland (111 per 100 000 inhabitants; 2011 data), as well as Ireland (licensed pharmacists), Malta, France, Greece (2011 data; professionally active), Spain, Lithuania (licensed pharmacists) and Italy (professionally active). The majority of the EU Member States reported 55–80 pharmacists per 100 000 inhabitants, although Denmark (45; 2009 data), Cyprus (23) and the Netherlands (21; 2011 data) were below this range.
Finland had the highest number of physiotherapists per 100 000 inhabitants
Physiotherapists (ISCO 08 code 2264) assess, plan and implement rehabilitative programs that improve or restore human motor functions, maximise movement ability, relieve pain syndromes, and treat or prevent physical challenges associated with injuries, diseases and other impairments. The relative distribution of physiotherapists across the individual EU Member States was more diverse than for dentists or pharmacists, ranging from 202 per 100 000 inhabitants in sparsely populated Finland (2011 data) down to 4 per 100 000 inhabitants in Romania.
Hospital beds
Hospital bed numbers provide information on the healthcare capacity of hospitals, in other words on the maximum number of patients who can be treated.
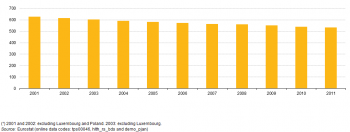
The number of hospital beds per 100 000 inhabitants averaged 534.9 in the EU-28 in 2011. The reduction in bed numbers between 2001 and 2011 across the whole of the EU-28 was equal to 92 fewer beds per 100 000 inhabitants. This reduction may reflect, among other factors, economic constraints, increased efficiency through the use of technical resources (for example, imaging equipment), a general shift from in-patient to out-patient operations, and shorter periods spent in hospital following an operation.
Germany had the highest number of hospital beds relative to population size
Among the EU Member States, this ratio ranged from 271 beds per 100 000 inhabitants in Sweden to 822 in Germany; among the non-member countries for which data are available Liechtenstein (215) and Turkey (253) were both outside this range. Note that for the United Kingdom only beds in public hospitals are included while the same is true in Ireland except that psychiatric care beds in the private sector are also included.
More than two thirds of all beds in EU-28 hospitals were for curative care
An analysis of the availability of hospital beds, identifying curative care beds, psychiatric care beds, long-term care beds and other hospital beds, is also provided in Table 4. In 2011, more than two thirds (67.7 %) of all beds in EU-28 hospitals were for curative care, 13.6 % for psychiatric care and the remaining 18.7 % for long-term care and other purposes.
The share of curative care beds among all hospital beds was highest in Cyprus (94 %), followed by Greece (84 %, 2009 data) and Portugal (83 %). In contrast, less than three fifths of hospital beds were for curative care in Hungary, Malta, France and Finland. The highest share of beds used for psychiatric care was 32 % in Malta, with shares over 25 % also recorded in the Netherlands (2009 data) and Belgium. In Cyprus, Hungary and Italy, 6 % or less of hospital beds were psychiatric care beds. In most EU Member States (no data for Germany, Greece, Portugal and the United Kingdom), long-term care beds accounted for 11 % or less of the total number of hospital beds, with Romania (12 %), Hungary (16 %), Estonia (22 %) and Finland (30 %) reporting higher shares.
Hospital discharges of in-patients and day care patients
Output-related indicators focus on hospital patients. Two such indicators are the number of hospital discharges (shown in this article for in-patients and day care patients) and the average length of stay for in-patients.
In 2012, there were in excess of 88 million discharges of in-patients (based on latest available data) in the EU-28, around 17.5 thousand per 100 000 inhabitants. There was a wide range in in-patient discharge rates between EU Member States in 2013 (see Figure 4). These peaked at 30.0 thousand discharges per 100 000 inhabitants in Bulgaria, while there were also relatively high numbers of discharges per 100 000 inhabitants in Austria (26.6 thousand) and Germany (24.4 thousand). By contrast, the lowest number of discharges per 100 000 inhabitants — below 10 thousand — were recorded in three of the southern EU Member States, namely, Spain, Portugal and Cyprus.
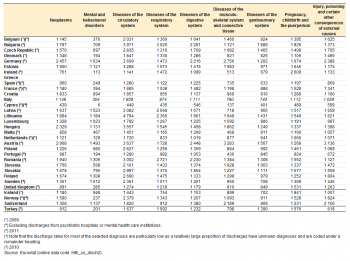
In nearly all Member States diseases of the circulatory system were the most common diagnosis among hospital discharges of in-patients
Diseases of the circulatory system were often the most common diagnosis among hospital discharges of in-patients (see Table 5). More than one quarter of the EU Member States for which data are available reported in excess of 3 000 discharges of in-patients per 100 000 inhabitants for diseases of the circulatory system. The Member States where other diagnoses were more common were Ireland and the United Kingdom where pregnancy, childbirth and the puerperium was the most common diagnosis. Note that for Cyprus the discharge rates for most of the selected diagnosis are particularly low as a relatively large proportion of discharges have unknown diagnoses and are coded under a remainder heading.
Among the EU Member States (leaving aside data for Cyprus), discharge rates for in-patients varied greatly for two of the diagnoses shown in Table 5: mental and behavioural disorders and diseases of the musculoskeletal system and connective tissue. It should be noted that for several Member States and for Norway discharges from psychiatric hospitals or mental health care institutions are excluded, thereby reducing the discharge rates for mental and behavioural disorders in particular.
For day care patients, the two most common diagnoses were diseases of the genitourinary system and neoplasms
In 2012, there were in excess of 31 million discharges of day care patients (based on latest available data) in the EU-28, around 6.2 thousand per 100 000 inhabitants. Relative to population size (see Table 6), the two most common diagnoses were diseases of the genitourinary system and neoplasms — reflecting the use of day care for some cancer treatments such as chemotherapy and some kidney disease treatments such as dialysis — although there were many exceptions (see Table 6).
Average length of stay of in-patients
Men generally had longer average lengths of stay as in-patients than women
The average length of a hospital stay as an in-patient ranged from 5.2 days in Denmark (2009 data) to 8.8 days in Austria (2011 data), with Portugal (2010 data) below this range and Finland, the Czech Republic (2011 data), Croatia, Hungary and Germany (2011 data) above it (see Table 7). The average length of stay for in-patients was generally longer for men than for women, with only Hungary, Belgium (2009 data) and Finland reporting the reverse situation; the largest gender difference was observed in Croatia, where men spent an average of 1.5 days more in hospital per stay.
With the exception of infants aged less than 1 year, the average length of stay was generally lowest for young children (aged 1–4 or 5–9) and increased with age. The longest average stays were recorded for one of the highest age groups, for persons aged 80–84, 85–89, 90–94 or 95 and over, with notable exceptions in Romania (2011 data) and Croatia where the longest stays were for persons aged 45–49 and 50–54 respectively. The increase in the average length of stay as age increases was most notable in Finland and Hungary: in Hungary the average length of stay ranged from 3.7 days for persons aged 1–4 to 30.6 days for persons aged 95 and over, while in Finland the range was from 2.8 days to 27.1 days for the same age groups.
The longest hospital stays for in-patients were nearly always for mental and behavioural disorders
Among the nine diagnoses presented in Table 8, the average length of stay for in-patients was notably longer for mental and behavioural disorders. Denmark (2009 data), France (2011 data) and Cyprus were the only EU Member States where there was a longer average length of stay for another diagnosis, reflecting the particularly low average lengths of stay for mental and behavioural disorders in these three Member States; note that in France and Cyprus, as well as in several other Member States and in Norway, the data presented in Table 8 exclude discharges from psychiatric hospitals or mental health care institutions. The longest average stays for in-patients with mental and behavioural disorders were reported for the Czech Republic, Malta (2011 data) and the United Kingdom (2011 data), all around 50 days. Among the other diagnoses, the average lengths of stay were generally highest for patients being diagnosed or receiving treatment for neoplasm (benign or malignant) or diseases of the circulatory system.
For several of the diagnoses shown in Table 8 there was a relatively high degree of uniformity in the average length of stay reported by each EU Member State. For example, in-patients diagnosed with neoplasms spent on average between 5.9 days (in Denmark; 2009 data) and 10.0 days (in Ireland) in hospital; patients diagnosed with diseases of the digestive system and those diagnosed with diseases of the genitourinary system also reported quite similar average lengths of stay across the Member States.
Data sources and availability
Eurostat, the Organisation for Economic Cooperation and Development (OECD) and the World Health Organisation (WHO) have established a common framework for a joint healthcare data collection. Following this framework, EU Member States submit their data to Eurostat on the basis of a gentlemen’s agreement. The data collected relates to statistics on human and physical resources in healthcare — supplemented by additional Eurostat data on hospital activities (discharges and procedures) — as well as healthcare expenditure following the methodology of the system of health accounts (SHA).
Non-expenditure healthcare data are mainly based on administrative national sources; a few countries compile this information from surveys. As a consequence, the information collected may not always be comparable. Information on the non-expenditure component of healthcare can be divided into two broad groups of data:
- resource-related healthcare data on human, physical and technical resources, including personnel (such as physicians, dentists, nursing and caring professionals, pharmacists and physiotherapists) and hospital beds;
- output-related data that focuses on hospital patients and their treatment(s), in particular for in-patients.
Hospitals are defined according to the classification of healthcare providers within the SHA; all public and private hospitals should be covered.
Note on tables: For cells which include symbol ':' data are not available.
Healthcare personnel — methodology
Statistics on healthcare resources — including personnel — are documented in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Common definitions have been agreed between Eurostat, the OECD and the WHO with respect to the employment of various health care professionals. Three main concepts are used to present this data; Eurostat gives preference to the concept of ‘practising’ health care professionals:
- ‘practising’, in other words, health care professionals providing services directly to patients;
- ‘professionally active’, in other words, ‘practising’ professionals plus health care professionals for whom their medical education is a prerequisite for the execution of their job;
- ‘licensed’, in other words, health care professionals who are registered and entitled to practise as health care professionals.
Data on personnel are classified according to the International Standard Classification of Occupations (ISCO): see codes 221 (medical doctors), 222, 322 and 532 (nursing and caring professionals) and 226 (including dentists, pharmacists and physiotherapists).
For country specific notes, please refer to these background information documents:
- physicians;
- physicians by speciality;
- dentists;
- nursing and caring professionals;
- pharmacists;
- physiotherapists.
Hospital beds — methodology
Statistics on healthcare resources — including beds in hospitals — are documented in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Hospital beds are those beds which are regularly maintained and staffed and immediately available for the care of admitted patients. Both occupied and unoccupied beds are included. Excluded are recovery trolleys and beds for same day care (day care and out-patient care), provisional and temporary beds. Hospital beds are presented for four categories:
- Curative care beds in hospitals are for patients where the principal clinical intent is to do one or more of the following: manage labour (obstetric), perform surgery, cure or treat (including relieving symptoms, reducing severity, or protecting against exacerbation and / or complication) of non-mental illness or injury, perform diagnostic or therapeutic procedures. Beds for palliative and long-term nursing care are recorded under long-term care.
- Psychiatric care beds in hospitals are for patients with mental health problems. Included are all beds in mental health and substance abuse hospitals, as well as beds in psychiatric departments of general and specialty hospitals. Beds for long-term nursing care in mental health and substance abuse hospitals are recorded under psychiatric care beds. Beds for palliative care are recorded under long-term care.
- Long-term care beds in hospitals are for patients requiring long-term care due to chronic impairments and a reduced degree of independence in activities of daily living, including palliative care.
- Other beds, including beds for rehabilitation.
The statistics should include public as well as private sector establishments — although some EU Member States provide data only for the public sector — for example, Denmark (psychiatric beds), Ireland (total and curative beds), Cyprus (curative and psychiatric beds) and the United Kingdom.
For country specific notes on this data collection, please refer to this background information document: hospital beds by type of care.
Hospital discharges and average length of stay — methodology
Statistics on healthcare activities — including discharges and average length of stay — are documented in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Output-related indicators focus on hospital patients and cover the interaction between patients and healthcare systems, generally through the form of the treatment they receive. Data are available for a range of indicators including hospital discharges of in-patients and day cases by age, gender, and selected (groups of) diseases; the average length of stay of in-patients; or the medical procedures performed in hospitals. The number of hospital discharges is the most commonly used measure of the utilisation of hospital services. Discharges, rather than admissions, are used because hospital abstracts for in-patient care are based on information gathered at the time of discharge.
For country specific notes on this data collection, please refer to this background information document: hospital discharges by diagnosis (ISHMT).
Context
Health outcomes across the EU are strikingly different according to where people live, their ethnicity, sex and socioeconomic status. In addition, the structure of healthcare services in the EU also varies in terms of funding, provision and organisational arrangements across countries and with respect to their public–private mix. The EU promotes the coordination of national healthcare policies through an open method of coordination which places particular emphasis on the access to, and the quality and sustainability of healthcare. Some of the main objectives include: shorter waiting times; universal insurance coverage; affordable care; more patient-centred care and a higher use of outpatients; greater use of evidence-based medicine, effective prevention programmes, generic medicines, and simplified administrative procedures; and strengthening health promotion and disease prevention.
Directive 2005/36/EC on the recognition of professional qualifications provides a Europe-wide legal framework enabling EU Member States to recognise each other’s qualifications. A range of health professionals — including doctors, dentists, pharmacists and physiotherapists — enjoy automatic recognition, in other words, if they are a certified practitioner in their home country then they are automatically entitled to practice anywhere else in the EU.
One consequence of ongoing and future demographic developments is that the number of elderly persons (aged 65 and over) in the EU-28 is forecast to increase by almost 60 % during the period 2014–54 (Eurostat; EUROPOP 2013 main scenario). The ageing of the EU’s population is likely to result in considerable demand for a range of age-related services, as an increasing proportion of the population becomes frail and suffers from declining physical and mental health. European healthcare systems will therefore need to anticipate needs for future skills in order to match the supply of health professionals, for example nurses and caring professionals, to the demands of an increasingly aged society, and to accommodate a probable shift away from care in hospitals towards care in the home. An action plan for the EU health workforce seeks to help EU Member States tackle the challenge of an increase in the demand for healthcare, by: improving workforce planning and forecasting; anticipating future skills’ needs; improving the recruitment and retention of health professionals; mitigating the negative effects of migration on health systems. The plan is part of the broader strategy ‘Towards a job-rich recovery’ (COM(2012) 173).
See also
Online publications
Healthcare human and physical resources
- Physicians
- Nursing and caring professionals
- Dentists, pharmacists and physiotherapists
- Beds
- Technical resources and medical technology
Healthcare activities
- Hospital discharges and length of stay
- Surgical operations and procedures
- Consultations
- Preventive services
- Medicine use
- Unmet needs for health care
Methodology
General health statistics articles
- Health statistics introduced
- Health statistics at regional level - healthcare resources
- Healthcare expenditure
- The EU in the world — health
Further Eurostat information
Main tables
Database
- Health care, see
- Health care resources (hlth_res)
- Health care activities (hlth_act)
Dedicated section
Methodology / Metadata
- Healthcare resources (ESMS metadata file — hlth_res)
- Healthcare activities (ESMS metadata file — hlth_act)
Source data for tables and figures (MS Excel)
External links
- European Commission — Directorate-General for Health and Food Safety — European Core Health Indicators (ECHI)
- European Commission — Directorate-General for Health and Food Safety — Health Systems Performance Assessment
- European Commission — Directorate-General for Health and Food Safety — Health workforce
- European Commission — Directorate-General for Health and Food Safety — Public health
- Joint OECD / European Commission report ‘Health at a Glance: Europe 2014’
- OECD — Health policies and data
- World Health Organisation (WHO) — Health systems [[Category:Health care>|Healthcare provision statistics]]

