Data extracted in March 2024.
Planned article update: April 2026.
Highlights
In 2021, Malta recorded the lowest standardised death rate for cancer among EU countries,
198.3 per 100 000 inhabitants.
In 2021, among the EU countries, the highest standardised death rates for cancer were recorded in Hungary and Croatia, each with rates above 300 per 100 000 inhabitants.
In-patient average length of stay for neoplasms, 2021
This article presents an overview of statistics related to cancer in the European Union (EU) and focuses on three aspects: deaths from cancer, cancer healthcare and the availability of specialist day care and equipment for the treatment of cancer. Some of the statistics presented in this article are only available for the broader category of neoplasms, which includes benign and uncertain neoplasms as well as malignant ones (cancer). An accompanying article, Cancer statistics – specific cancers, looks in more detail at statistics for a selection of specific cancers: colorectal cancer, lung cancer, breast cancer and prostate cancer.
This article is one of a set of statistical articles concerning health status in the EU which forms part of the online publication on Health in the European Union - facts and figures.
Deaths from cancer
In 2021, cancer was the second leading cause of death in the EU, with 1.1 million deaths, which equated to 21.6 % of the total number of deaths in the EU – see Table 1. Cancer accounted for a higher share (23.8 %) of deaths among males than among females (19.4 %).
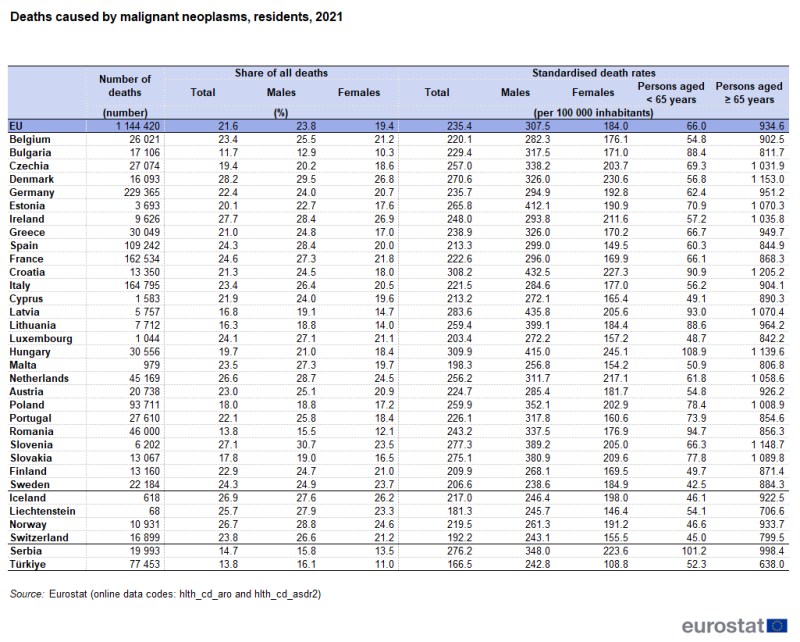
Source: Eurostat (hlth_cd_aro) and (hlth_cd_asdr2)
Among the EU countries, the share of deaths from cancer in the total number of deaths in 2021 reached or exceeded 26.0 % in Denmark (28.2 %), Ireland (27.7 %), Slovenia (27.1 %) and the Netherlands (26.6 %). Among males, this share peaked at 30.7 % in Slovenia, followed by 29.5 % in Denmark. Among females, it peaked at 26.9 % in Ireland, followed by 26.8 % in Denmark. By contrast, less than 16.0 % of all deaths in Romania (13.8 %) and Bulgaria (11.7 %) were caused by cancer.
In the EU, the standardised death rate for cancer was 235.4 per 100 000 inhabitants in 2021, lower than the rate for circulatory diseases, but higher than the rate for other causes of death, including COVID-19. The article causes of death statistics looks in more detail at the leading causes of death in the EU.
An analysis by sex and by age shows large differences in standardised death rates for cancer: for males the rate (307.5 per 100 000 male inhabitants) was 67 % higher than that for females (184.0 per 100 000 female inhabitants), while the rate for persons aged 65 years and over was 14 times as high as it was for younger persons (those aged less than 65 years).
Among the EU countries, the highest standardised death rates for cancer were recorded in Hungary and Croatia, both with rates over 300.0 per 100 000 inhabitants in 2021. For males, the highest standardised death rates for cancer were reported in Latvia and Croatia, both with rates above 430.0 per 100 000 male inhabitants. For females, the highest standardised death rates for cancer were recorded in Hungary, Denmark and Croatia, each with rates over 220.0 per 100 000 female inhabitants.
In 2021, Malta recorded the lowest standardised death rate for cancer among the EU countries, 198.3 per 100 000 inhabitants, and was the only country with a rate below 200.0 per inhabitant. Sweden recorded the lowest standardised death rates among males: 238.6 per 100 000 male inhabitants. Spain had the lowest standardised death rate among females: 149.5 per 100 000 female inhabitants.
Cancer healthcare activities
This section covers three sets of data that are available for cancer healthcare. These concern the number of discharges of in-patients, the average length of stay for in-patients, and the type of operations and procedures performed.
Concerning the provision of care, this article concentrates on in-patient care, day care and surgical procedures. Both in-patient care and day care comprise a formal admission into a healthcare facility such as a hospital for diagnosis, treatment or other types of healthcare. While in-patient care involves an overnight stay after admission, day care comprises planned medical and paramedical services delivered to patients without an overnight stay: day care patients are formally admitted with the intention of being discharged on the same day. The inclusion of accommodation with medical and ancillary care constitutes the main distinction between in-patient and outpatient care.
In 2021, there were around 5.9 million in-patients in the EU who were discharged from hospitals having been treated for neoplasms (including 2020 data for Malta and excluding Denmark, Greece and Luxembourg).
Austria recorded the highest discharge rate for in-patients with neoplasms
Figure 1 shows that, for all neoplasms, the highest discharge rate for in-patients was in Austria, where 2 584 in-patients per 100 000 inhabitants were discharged in 2021 after diagnosis or treatment. In Germany and Bulgaria this rate also exceeded 2 000 per 100 000 inhabitants. Elsewhere the rate ranged from 1 830 per 100 000 inhabitants in Croatia to 769 per 100 000 inhabitants in Portugal, with Ireland and Malta (2020 data) below this range.
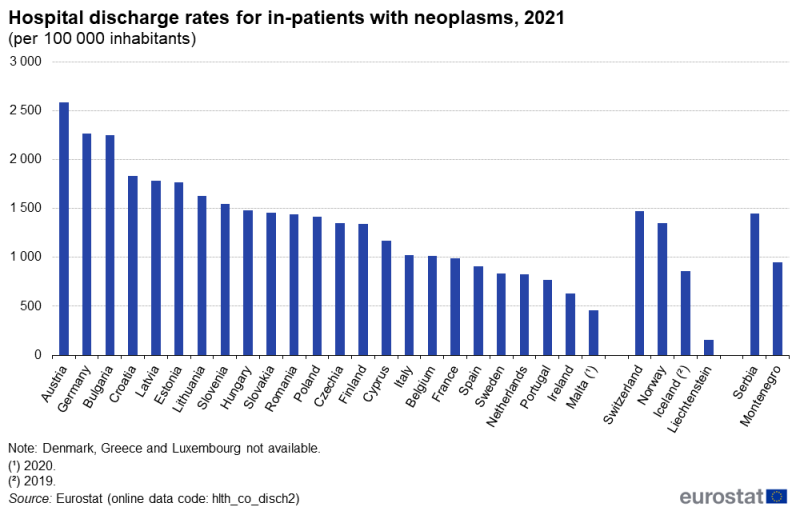
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)
Neoplasms: falling average length of stay for in-patients
The average length of stay in 2021 for in-patients having been classified for the purpose of their treatment or investigation under neoplasms ranged among the EU countries from 4.6 days in Bulgaria and Cyprus to 11.5 days in Malta (no recent data for Denmark, Greece or Luxembourg). A comparison of the data for 2021 with that for 2016 (see Figure 2 for the precise availability) shows an overall downward pattern in the average length of stays for in-patients. Increases were recorded only for Malta (up 2.5 days between 2016 and 2020) and Estonia (up 0.1 days). The largest reduction in terms of the average length of stay was recorded in Cyprus with 2.4 fewer days in 2021 than in 2016.
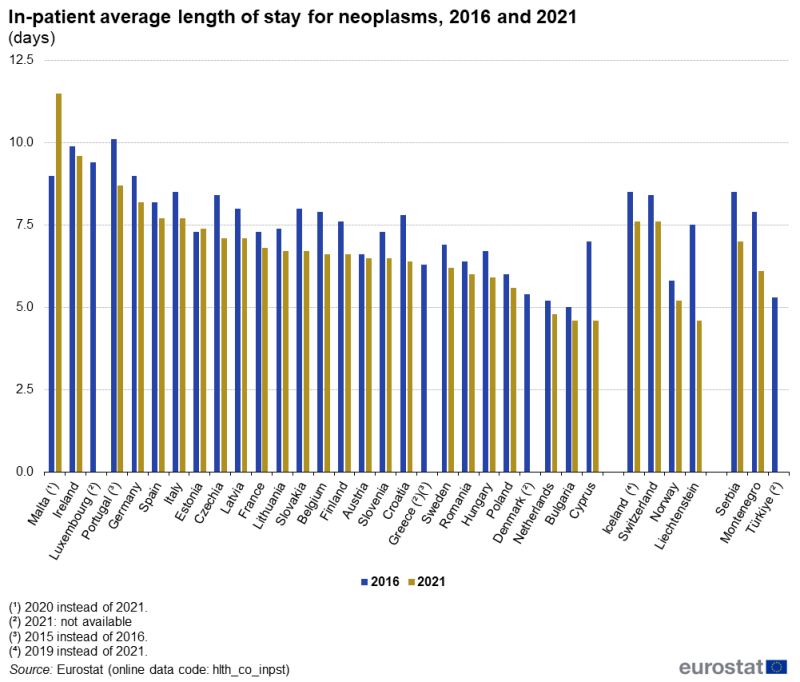
(days)
Source: Eurostat (hlth_co_inpst)
Table 2 presents data for the frequency (relative to population size) with which two procedures were carried out to prevent or treat breast cancer: the removal of part (partial excision of mammary gland) or all (total mastectomy) of a mammary gland. In 2021, 363 000 operations were performed in the 24 EU countries for which data are available (2020 data for Malta, 2019 data for the Netherlands, no data for Czechia, Greece or Slovakia) to remove part of a mammary gland. A further 141 000 total mastectomies were performed in 25 countries (similar coverage but including data for Slovakia).
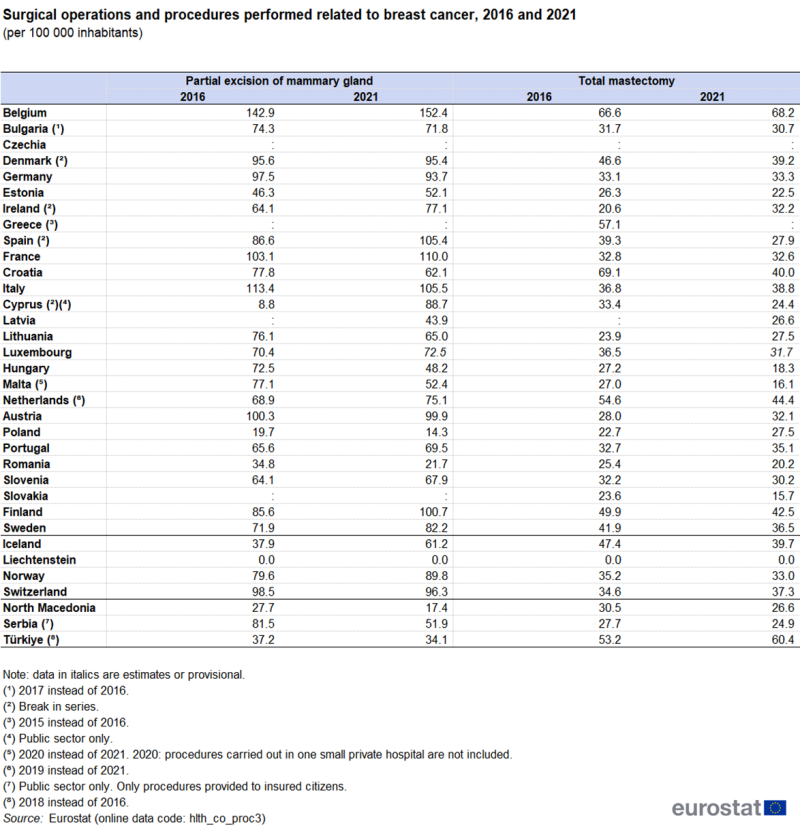
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_proc3)
In 2021, partial mastectomies were most commonly performed in Belgium, with 152.4 of these procedures per 100 000 inhabitants, while the next highest rate was in France with 110.0 procedures per 100 000 inhabitants. Poland and Romania recorded the lowest frequencies for this procedure, with, respectively, 14.3 and 21.7 partial mastectomies per 100 000 inhabitants. Total mastectomies were most common in 2021 in Belgium with 68.2 total mastectomies per 100 000 inhabitants. The Netherlands (2019 data), Finland and Croatia also recorded more than 40.0 total mastectomies per 100 000 inhabitants.
Relative to population size, the majority of EU countries recorded a decrease in the frequency of mastectomies
For partial mastectomies, around half of the EU countries for which data are available reported a decrease in the frequency of this operation between 2016 and 2021. The largest decreases were reported by Romania (down 38 %), Hungary (down 34 %), Malta (down 32 %; 2016 to 2020) and Poland (down 27 %). The largest increases between 2016 and 2021 were observed in Cyprus, Spain and Ireland, but all had a break in series. The next largest increase was recorded in Finland, up 18 %.
For total mastectomies, 16 EU countries recorded decreases between 2016 and 2021, with the largest in Croatia (down 42 %). After Ireland (which had a break in series), the largest increase was in Poland (up 21 %).
Oncological day care involves treatments that do not require an overnight stay, for example day case chemotherapy, blood and platelet transfusions, tests, removal of sutures (stitches), injections and dressings. Although only a limited amount of data is available (see Table 3 for data availability), the range in availability of day care places in 2021 was large, from 0.2 places per 100 000 inhabitants in Slovakia to 15.6 places per 100 000 inhabitants in Belgium and 21.1 places per 100 000 inhabitants in Spain.
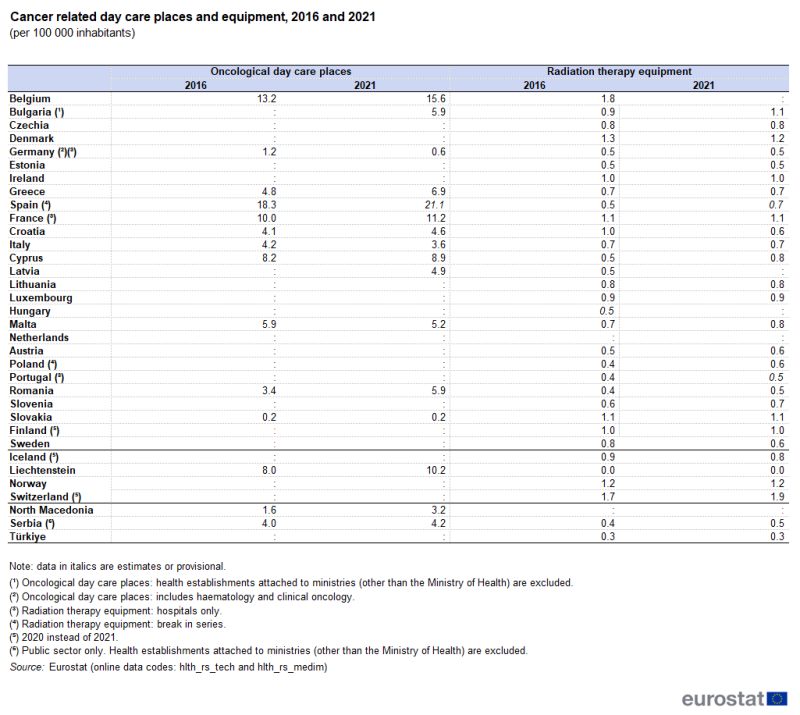
(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_tech) and (hlth_rs_medim)
Radiation therapy equipment covers machines used for treatment with x-rays or radionuclides. These include linear accelerators, Cobalt-60 units, Caesium-137 therapy units, low to orthovoltage x-ray units, high dose and low dose rate brachytherapy units, and conventional brachytherapy units: note that some of these machines may also be used for treatments other than for cancer. In 2021, there were 2 976 radiation therapy units in the EU countries for which data are available (2020 data for Finland; no data for Belgium, Latvia, Hungary and the Netherlands; note that data for Germany, France and Portugal refer only to equipment in hospitals), with the largest numbers in France (775), Italy (432) and Germany (398). Relative to population size, radiation therapy equipment was most common in Denmark (1.2 per 100 000 inhabitants), while it was least common in Romania, Portugal (hospitals only), Germany (hospitals only) and Estonia all (0.5 per 100 000 inhabitants).
Source data for tables and graphs
Key concepts
Data sources
An in-patient or day care patient is discharged from hospital when formally released after a procedure or course of treatment (episode of care). A discharge may occur because of the finalisation of treatment, signing out against medical advice, transfer to another healthcare institution, or because of death.
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised (rather than crude) death rate can be compiled which is independent of the age and sex structure of a population: this is done as most causes of death vary significantly by age and according to sex and the standardisation facilitates comparisons of rates over time and between countries.
Statistics on causes of death provide information on mortality patterns, supplying information on developments over time in the underlying causes of death. This source is documented in more detail in the background article Causes of death statistics – methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Causes of death are classified according to the European shortlist (86 causes), which is based on the International Statistical Classification of Diseases and Related Health Problems (ICD). Chapter II of the ICD covers neoplasms.
- C00-C97 Malignant neoplasms
- D00-D09 In situ neoplasms
- D10-D36 Benign neoplasms
- D37-D48 Neoplasms of uncertain or unknown behaviour
Please refer to national reference metadata for more information.
Standardised death rate
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised death rate is adjusted to a standard age distribution. This facilitates comparisons of rates over time and between countries. The European standard population used for the standardisation of crude rates is based on the European Standard Population (ESP) in use since the summer of 2013. For hospital discharges and the length of stay in hospitals, the International Shortlist for Hospital Morbidity Tabulation (ISHMT) is used to classify data from 2000 onwards; Chapter II covers neoplasms.
- Malignant neoplasm of colon, rectum and anus (0201)
- Malignant neoplasms of trachea, bronchus and lung (0202)
- Malignant neoplasms of skin (0203)
- Malignant neoplasm of breast (0204)
- Malignant neoplasm of uterus (0205)
- Malignant neoplasm of ovary (0206)
- Malignant neoplasm of prostate (0207)
- Malignant neoplasm of bladder (0208)
- Other malignant neoplasms (0209)
- Carcinoma in situ (0210)
- Benign neoplasm of colon, rectum and anus (0211)
- Leiomyoma of uterus (0212)
- Other benign neoplasms and neoplasms of uncertain or unknown behaviour (0213)
Statistics on healthcare resources (such as personnel and medical equipment) and healthcare activities (such as information on surgical operations and procedures and hospital discharges) are documented in the background article Healthcare non-expenditure statistics – methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For surgical operations and procedures the International Classification of Diseases – clinical modification (ICD-9-CM) is used.
- Partial excision of a mammary gland (85.20-85.23)
- Total mastectomy (85.33-85.36 and 85.4)
Note on tables:
- a colon ‘:’ is used to show where data are not available;
- a dash ‘–’ is used to show where data are not applicable/relevant.
Context
Although significant advances have been made in the fight against this group of diseases, cancer remains a key public health concern and a tremendous burden on EU societies – it is the second largest cause of death in the EU.
Europe’s Beating Cancer Plan, presented in February 2021, is the EU’s response to growing challenges and developments in cancer control and represents a political commitment ‘to leave no stone unturned in the fight against cancer’. Built around 10 flagship initiatives and several supporting actions, it forms part of the European Commission’s proposals for a strong European Health Union, with a view to ensuring a more secure, more resilient and better-prepared EU.
Europe’s Beating Cancer Plan supports EU countries’ work to prevent cancer and to ensure a high quality of life for cancer patients, survivors, their families and carers. It is structured around a number of key areas where the EU can add most value:
- prevention,
- early detection,
- diagnosis and treatment,
- quality of life of cancer patients and survivors.
Explore further
Other articles
Online publications
Health status – selected diseases and related health problems
Causes of death
Healthcare activities
Methodology
General health statistics articles
Database
- Health (hlth), see:
- Health care (hlth_care)
- Health care resources (hlth_res)
- Health care staff (hlth_staff)
- Health care facilities (hlth_facil)
- Health care activities (hlth_act)
- Hospital discharges and length of stay for inpatient curative care (hlth_co_inpagg)
- Hospital discharges - national data (hlth_hosd)
- Length of stay in hospital (hlth_hostay)
- Operations, procedures and treatment (hlth_oper)
- Health care resources (hlth_res)
- Causes of death (hlth_cdeath)
- General mortality (hlth_cd_gmor)
- Causes of death - deaths by country of residence and occurrence (hlth_cd_aro)
- Causes of death - standardised death rate by NUTS 2 regions of residence (hlth_cd_asdr2)
- General mortality (hlth_cd_gmor)
- Health care (hlth_care)
Thematic section
Publications
Methodology
- Causes of death statistics (ESMS metadata file – hlth_cdeath_sims)
- Healthcare resources (ESMS metadata file – hlth_res)
External links
Selected datasets
- Health (t_hlth), see:
- Health care (t_hlth_care)
- Causes of death (t_hlth_cdeath)
