Archive:Causes of death statistics at regional level
- Data from March 2011, most recent data: Further Eurostat information, Main tables and Database.
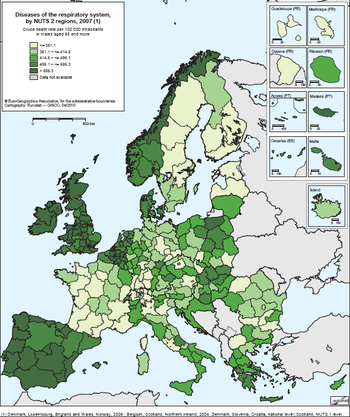
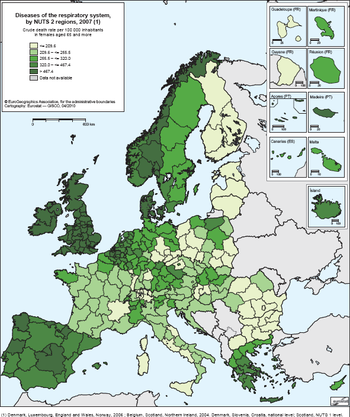
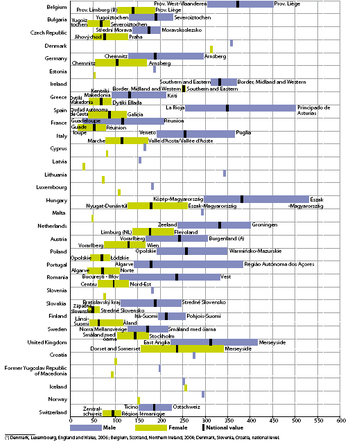
This article takes a look at mortality patterns in the European Union (EU), down to the regional level (NUTS 2). These vary significantly with age and gender, but also between countries and regions. Three types of factor determine mortality: intrinsic factors, such as age and gender; extrinsic factors, such as biological or collective social factors, living or working conditions; and individual factors, such as lifestyle, smoking, alcohol consumption, driving and sexual behaviour.
As a general rule, the mortality rate is higher among men than among women in all age groups. Although there are signs that the mortality gap is narrowing in some Member States, there are still significant differences between genders.
Main statistical findings
Causes of death — malignant neoplasms
Causes of death data give information on diseases leading directly to death, so they can be used as an indicator to plan health services. In the EU-27, the major cause of death was disease of the circulatory system but in France cancer took the lead, with 3 717 more deaths for the average period 2006–08.
In the Netherlands, cancer was also higher than circulatory system diseases, with 661 more deaths in the average period 2007–09.
Looking at the 27 Member States, the three-year average standardised death rate for 2006–08 for all malignant neoplasms show that the highest rates were in Hungary (240.9), Poland (207.7) and the Czech Republic (205.7). The lowest rates were in Cyprus (120.4), Finland (138.6) and Portugal (153.3). Analysing the data by gender, for men, Lithuania and Estonia had the second and third highest rates while Germany had one of the lowest. For women, Ireland has one of the highest rates of malignant neoplasms, in particular of the larynx, trachea, bronchus and lung and breast cancer, while Spain has one of the lowest.
Combined malignant neoplasms of the larynx, trachea, bronchus and lung
The form of cancer with highest death rates in all Member States, for all ages and both sexes, is combined malignant neoplasms of the larynx, trachea, bronchus and lung, with a three-year-average standardised death rate in 2006–08 of 39.6 per 100 000 inhabitants. The highest rates are in Hungary (68.4), Poland (54.9) and the Netherlands (47.3) and the lowest rates are in Cyprus (20.5), Portugal (26.0) and Finland (26.6).
Analysing the data by gender, the 2006–08 three-year-average standardised death rate for all ages for men is 65.8 in the EU-27. The highest rates are in Hungary (114.3), Poland (100.4) and Estonia (90.7). For women, the three-year-average standardised death rate is 18.9 per 100 000 inhabitants in the EU-27. Again, Hungary had the highest rate (35.7) followed by the Netherlands (31.7) and Ireland (28.6). The lowest rates are in Cyprus (7.7), Portugal (8.2) and Lithuania (8.6).
The regions with the highest rates are Eszak-Alfold (80.7), Eszak-Magyarorszag (71.9) and Del-Dunantul (71.7) in Hungary. The lowest rates were found in the French regions of Martinique (13.3), Guadeloupe (13.6) and Guyane (13.8). Analysing the data by gender, the Hungarian regions again had high death rates, followed by the Polish region of Warminsko-Mazurskie (127.0) for men and Flevoland (36.4) for women. The lowest rates for women are the Italian regions of Molise (5.8), Basilicata and Calabria (5.9).
The data can be analysed by age group using the crude death rate. The annual 2008 crude death rate shows that the highest rate was in the age group 80–84 (216.5), followed by 75–79-year-olds, with a rate of 258.3. Some countries, like Latvia, Romania, Slovenia and Slovakia, had higher rates in the age group 70–74. Amongst men, Bulgaria had the highest rate in the younger age group 65–69 (329.5).
Breast cancer
The three-year-average standardised death rate shows that for the EU-27, in all ages and both sexes, breast cancer, together with malignant neoplasms of the colon, was the second largest cause of death by cancer, with 13.3 deaths by 100 000 inhabitants. For women, this was the main cause of death in most Member States, with a rate of 23.9 per 100 000 inhabitants; for men the rate is 0.3. Exceptions are Hungary, the Netherlands and Poland, where this form of cancer is second to malignant neoplasms of the larynx, trachea, bronchus and lung. The highest rates of breast cancer for women are in Ireland (29.7), the Netherlands (28.9) and Hungary (26.7) while Spain (18.4), Portugal (19.6), and Finland (20.9) have the lowest rates.
For women, the most-affected regions are Friesland (35.9) in the Netherlands, Trier in Germany (31.7) and Bucureşti - Ilfov in Romania (31.3). The lowest rates were found in the French Réunion (14.1), Cantabria in Spain (15.2) and Ionia Nisia in Greece (15.3). For men, the region with the highest rate is Ciudad Autonoma de Ceuta (1.1).
An analysis of the 2008 crude death rate for women in the EU-27 by age group shows that breast cancer increases with age and that women over 85 are the most affected, with a rate of 223.8 per 100 000 inhabitants. In this age group, the highest rates were in Slovenia, Greece and Ireland and the lowest rates were in Romania, Lithuania and Bulgaria.
Malignant neoplasms of the prostate
Another gender-related form of cancer is malignant neoplasm of the prostate. For men in the EU-27, the three-year-average standardised death rate (2006–08) is 21.4, compared to 230.1 for all malignant neoplasms. Prostate cancer is the second most common cause of death for males in EU-27 countries. High rates are found in Lithuania (36.4), Latvia (34.7), Estonia (33.7) and Slovenia (33.2), with the lowest in Romania (15.1), Italy (16.0), Bulgaria (16.9) and Spain (17.6).
The most affected regions are the French Martinique (47.0) and Guadeloupe (41.1) and the Finish Åland (44.2). The lowest rates are found in the Romanian regions of Sud-Vest Oltenia (10.2) and Sud - Muntenia (10.8) and the Spanish Ciudad Autonoma de Melilla (10.5).
From 2000 to 2008, the crude death rate for males in the EU-27 of all ages increased in 2007 (28.3) and 2008 (28.4). The countries with highest rates in 2008 were Estonia (40.5), Latvia (35.5) and Portugal (34.3) and the lowest rates were in Romania (16.6), Slovakia (19.1) and Luxembourg (19.4). Estonia had the highest increase (from 31.7 to 40.5) and Luxembourg saw a marked decrease from 24.8 to 19.4.
The rate of prostate cancer increases with age. People aged 85 + have the highest rates, 657.0, for the EU 27. In general, prostate cancer starts to be a problem around the age of 50.
Hospital discharges
Regional data on hospital discharges of in-patients were not available until 2005 and not all countries are yet in a position to provide this data at subnational level.
Alongside information on the different ‘causes of death’, data on hospital discharges at national and regional levels are complementary means of estimating the frequency of treatment of some lethal diseases such as specific forms of malignant neoplasm.
On average, around 18 000 per 100 000 inhabitants and per country were discharged from hospitals in the EU-27 in 2008. However, that number hides a wide range of variations between countries, from 9 500 in Malta to over 27 500 in Austria.
A comparison of the number of in-patient discharges at NUTS level 2 indicates that regions in central Europe have the highest number of discharges per 100 000 inhabitants.
Malignant neoplasms of trachea, bronchus and lung
The above observation on central Europe also applies to combined malignant neoplasms of the trachea, bronchus and lung. In principle, the area stretching from Germany in the west to Romania in the east and from Croatia in the south to Denmark in the north has higher rates of in-patients per 100 000 inhabitants than other areas of the EU.
For the age group 70–74, Austria reports the highest figures (938 in-patient discharges per 100 000 inhabitants), with Hungary in second place (with 868) and Malta the lowest number (69). There is a similar pattern in the next age group (75–79), with Austria and Malta again recording the highest and lowest figures.
Out of the countries that provide regional data, Germany, the Czech Republic and, to a lesser degree, France show the greatest internal variability. In Bremen (Germany), 400 in-patients per 100 000 inhabitants were discharged, compared to barely 166 in Rheinland-Pfalz. Similarly, the ratio of Praha in the Czech Republic (205) is more than twice that in Strední Cechy. In France, the figures for Corse are very different from the mainland regions (121, twice the French average). The data for Germany and the Czech Republic are 2006 figures.
Breast cancer
Another major malignancy causing hospital stays and discharges is the gender-associated breast cancer. Again, the rates are highest in central Europe, followed by Finland and the Baltic States.
The population of women aged 40 to 44 can be considered as a ‘turning point’ for the risk of breast cancer. In all countries, this cohort is the first to record a high number of in-patient discharges. The same phenomenon is found at regional level. For this age group, Austria has the highest rate, with 485 per 100 000 inhabitants, Germany reports 352, and Malta has the lowest with 32.
Looking at the two age groups 70–74 and 75–79, once again Austria and Malta have the highest and lowest rates of all countries, just as they had for combined malignant neoplasms of the trachea, bronchus and lung. Austria recorded a rate of 1 164 discharges per 100 000 inhabitants for persons 70–74 years old, whilst the rate in Malta was only 101.
Germany and Austria also show important regional disparities when aggregating all female age groups. In Germany, Niedersachsen had a rate of 684 in-patient discharges per 100 000 inhabitants, but it was 1 229 in Schleswig-Holstein. In Austria, the difference is even bigger: as compared to Burgenland with only 626, Wien had a rate of 1919. Again, the data for Germany are from 2006.
Conclusion
Information on hospital discharges and causes of death are a prerequisite for monitoring the performance of health policy.
Regional indicators provide an insight into similarities, particularities and differences across regions in Europe.
There can be big differences between regions in the same country, and regions in different countries may be very similar. A thorough analysis of trends and variations in health indicators at regional level is therefore essential to plan and monitor action and programmes, formulate new policies, develop new strategies and contribute to evidencebased health policymaking.
Eurostat’s work on health statistics mainly focuses on further improvements that are needed to make the current data more comparable and complete and to extend regional coverage.
Data sources and availability
Cause of death (COD) statistics are based on information from death certificates. COD statistics record the underlying cause of death, i.e. to quote the definition adopted by the World Health Assembly, ‘the disease or injury which initiated the train of morbid events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury’.
In addition to absolute numbers, crude death rates and standardised death rates for COD are provided at national and regional levels. Regional-level data are provided in the form of three-year averages, along with yearly crude death rates for some age groups. The crude death rate (CDR) indicates mortality in relation to the total population. It is expressed per 100 000 inhabitants, i.e. calculated as the number of deaths recorded in the population over a given period divided by the population in the same period and then multiplied by 100 000. Crude death rates are calculated for five-year age groups.
However, the CDR is strongly influenced by the population structure. In a relatively ‘old’ population there will be more deaths than in a ‘young’ one because mortality is higher in older age groups. For comparisons, the age effect can be taken into account by using a standard population. The standardised death rate (SDR) is a weighted average of age-specific mortality rates. The weighting factor is the age distribution of a standard reference population. The ‘standard European population’ defined by the World Health Organisation (WHO) is used for this purpose. Standardised death rates are expressed per 100 000 inhabitants and calculated for the 0–64 age group (‘premature death’), 65+ and for all ages. Causes of death are classified into the 65 on the ‘European shortlist’, which is based on the international statistical classification of diseases and related health problems (ICD) developed and maintained by the WHO.
Hospital discharges are the formal release of a patient from a hospital after a procedure or course of treatment. They occur any time a patient leaves hospital upon completion of treatment, signing out against medical advice, transferring to another healthcare institution or death. A discharge includes in-patients and day cases but excludes transfers to another department within the same institution.
In-patients are patients who are formally admitted (or ‘hospitalised’) to an institution for treatment and/or care and stay for a minimum of one night or more than 24 hours in the hospital or other institution providing in-patient care.
Context
Health is an important priority for Europeans, who expect to be protected against illness and disease at home, in the workplace and when travelling across the EU. Health issues cut across a range of topics — including consumer protection (food safety issues), safety at work and environmental and social policies — and thus have a considerable impact on the EU’s revised Lisbon strategy.
Member States generally have the responsibility for organising and delivering health services and healthcare. The EU has the responsibility to give added value by launching initiatives such as those on cross-border health threats and patient mobility, reducing health inequalities and addressing key health determinants. Gathering and assessing accurate, detailed information on health issues is vital for the EU to effectively design policies and target future action.
On 23 October 2007, the European Commission adopted a new strategy ‘Together for health: A strategic approach for the EU 2008–13’ to set objectives that will guide future work on health at European level. Within the European Commission, the strategy is supported by the ‘Second programme of community action in the field of health 2008–13’. This programme has been adopted with three broad objectives that align future act on on health more closely to the objectives of prosperity, solidarity and security, namely:
- improving citizens’ health security;
- promoting health to improve prosperity and solidarity;
- generating and disseminating health knowledge.
To monitor progress on these objectives, Regulation 1338/2008 of the European Parliament and of the Council on Community statistics on ‘public health and health and safety at work’ is the legal framework for compiling the required background statistics. It covers causes of death, health status, health determinants and healthcare.
Further Eurostat information
Publications
- Eurostat regional yearbook 2010, chapter 12 (available in English, French and German)
- Eurostat regional yearbook 2011, chapter 5
Main tables
- Public health
- Main tables
- Public health (t_hlth)
- Causes of death (t_hlth_cdeath)
- Public health (t_hlth)
- Main tables
Database
- Health, see:
- Public health
- Database
- Public health (hlth)
- Causes of death (hlth_cdeath)
- Public health (hlth)
- Database
Dedicated section
- Health, see:
- Public health