Archive:Amenable and preventable deaths statistics
Data from June 2017. Most recent data: Further Eurostat information, Main tables and Database. Planned article update: June 2018
This article presents statistics on two different indicators of avoidable mortality: amenable and preventable deaths. The concept of amenable and preventable mortality is based on the idea that certain deaths (for specific age groups and according to specific diseases as defined by the ICD classification, see the section data sources and availability ) could be 'avoided', that means would not have occurred at this stage, if there had been more effective public health and medical interventions in place.[1] A death can be considered as amenable if it could have been avoided through optimal quality health care. The concept of preventable deaths is broader and includes deaths which could have been avoided by public health interventions focusing on wider determinants of public health, such as behaviour and lifestyle factors, socioeconomic status and environmental factors.
Assessing the performance of health care systems is of increasing importance in the EU. While amenable and preventable mortality indicators are not meant to be a definite measurement of the quality of the health care in Member States, they provide some indication for the quality and performance of health care and (wider) public health policies in a country. In addition to health care and public health policies, other factors related to the likelihood of individuals to contract a disease or to seek medical advice - such as education, social class, health beliefs, levels of concerns, costs of diagnosis and treatment - are likely to influence the amount of amenable and preventable deaths in countries.[2] Improvements in health policies should translate into lower values for amenable and preventable deaths. However, there is likely to be a long time lag between implementation of health (care) policies and changes in the mortality rates, and hence conclusions need to be drawn with caution.
In 2014, over 562 000 deaths in the EU could have potentially been avoided with health care systems offering timely and effective medical treatments (amenable deaths) and close to 1 million deaths could have been prevented through better public health interventions (preventable deaths). The total number of potentially avoidable deaths - which accounts for the fact that certain diseases are both preventable and amenable – reached nearly 1.2 million in 2014[3]. The leading cause of avoidable mortality was ischaemic heart diseases.
This article is one of a set of statistical articles concerning health status in the EU which forms part of an online publication on health statistics.

(per 100 000 inhabitants)
Source: Eurostat (hlth_cd_apr)

(number)
Source: Eurostat (hlth_cd_apreu)

(per 100 000 inhabitants)
Source: Eurostat (hlth_cd_apr)
(numbers)
Source: Eurostat (hlth_cd_apreu)
(number)
Source: Eurostat (hlth_cd_apreu)
(% of total deaths)
Source: Eurostat (hlth_cd_apreu)
(% of total deaths)
Source: Eurostat (hlth_cd_apreu)
Main statistical findings
In 2014, deaths from potentially avoidable causes in the EU amounted to 562 000
In the European Union (EU), 1.7 million persons aged less than 75 years died in 2014. Among them, over 562 000 deaths (or 126 deaths per 100 000 inhabitants) could have been avoided in the light of better healthcare systems (amenable deaths). The change compared to 2013 is negligible, showing that these figures are rather stable in the short run. Across EU Member States a substantial number of deaths can be considered as potentially avoidable and variations depend on Member States' population size. Table 1 shows data for standardized death rates of amenable mortality, which takes into account the population structure of countries. Among EU Member States, the lowest amenable mortality rates in 2014 are found for France, Luxembourg, the Netherlands and Spain. On the other end of the spectrum are Latvia, Romania, Lithuania and Bulgaria, with high rates of potentially amenable deaths.
…and nearly a million deaths could have been prevented by public health interventions.
The figures for preventable mortality are higher than those for amenable mortality, due to the broader definition of preventable deaths (Data sources and availability) (see Table 1). In 2014, close to 1 million deaths (or 214 deaths per 100 000 inhabitants) could have been prevented through better public health interventions (see Table 2). These figures are again very similar to 2013 data. The Member States with the lowest preventable mortality rates in 2014 are Italy, Cyprus, Spain and Malta; while Member States with the highest levels of potentially preventable deaths are Lithuania, Latvia, Hungary and Romania.
The total number of deaths that could have potentially been avoided through effective public health and medical interventions reached nearly 1.2 million in 2014 (Table 2). [4]
Amenable mortality rates are higher for men than for women in Europe
Consistently throughout Europe, amenable mortality rates for men are higher than those for women (see Figure 1). The smallest gender gaps (compared to the total amenable mortality rate) are observed for the Netherlands, France, Denmark and Belgium. Similar results are obtained for preventable mortality rates (not shown in this article).
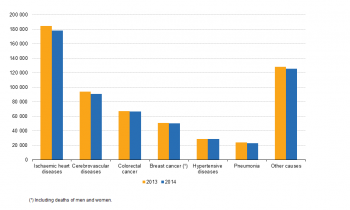
Heart diseases is the leading cause of amenable and preventable deaths
As shown in Figure 2, the six leading causes of amenable mortality are the following diseases or conditions (with decreasing importance): ischaemic heart diseases, cerebrovascular diseases, colorectal cancer, breast cancer, hypertensive diseases and pneumonia (a full overview of the diseases and conditions included in amenable mortality is presented in Table 2). In total, over 77 % of all deaths classified as amenable in the EU were caused by the aforementioned diseases. Heart diseases alone accounted for over 31 % of amenable deaths. As can be seen in Figure 2, the distribution across these diseases remained stable in the two periods studied, where all causes of death had a slight decrease with the exception of pneumonia which had a slight increase.
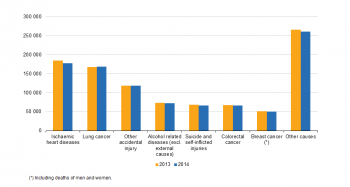
The leading causes for preventable deaths are lung cancer, injuries and alcohol related diseases
Over 73 % of preventable deaths in the EU are attributable to the following diseases and conditions (with decreasing importance): ischaemic heart diseases, lung cancer, accidental injuries, alcohol related diseases, colorectal cancer, suicides and self-inflicted injuries and breast cancer (a full overview of the diseases and conditions included in preventable mortality is presented in Table 2). Again, the split of deaths over these diseases remained stable in the two periods studied (see Figure 3).
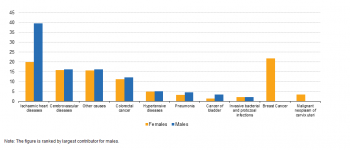
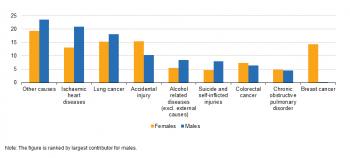
Similar leading causes of amenable mortality for men and women, with the exception of breast and cervical cancer for women
The distribution of diseases and conditions causing both amenable and preventable deaths varies slightly for men and women. While for men the leading cause of amenable mortality in percentage terms is ischaemic heart diseases, for women it is breast cancer (Figure 4). For preventable mortality, the leading cause for men is again ischaemic heart diseases, while accidental injuries and breast cancer are equally important causes of preventable deaths for women (Figure 5).
Data sources and availability
The definitions of amenable and preventable death are as follows[5]:
- A death is amenable if, in the light of medical knowledge and technology at the time of death, all or most deaths from that cause could be avoided through optimal quality health care.
- A death is preventable if, in the light of understanding of the determinants of health at the time of death, all or most deaths from that cause could be avoided by public health interventions in the broadest sense.
To calculate amenable and preventable mortality, one has to define, in a first step, which diseases and conditions could have been potentially avoided through optimal quality health care (amenable deaths) and through public health interventions (preventable deaths). To do this, Eurostat set up a Task Force composed of health care experts to define a list of precise conditions and diseases, which in the light of the current medical knowledge and technology could have been avoided. The complete list of diseases and conditions counted in either amenable or preventable deaths can be found here. The list also includes specifications on the age up to which a death can be considered as either amenable or preventable. The main age limit is set at 74 years to reflect the current life expectancy. In addition, for certain deaths the age limit is lower due to uncertainties in the treatment of the diseases. For example, if an individual aged below 50 years suffers from diabetes, then timely health care is very likely to be effective in preventing that this individual dies of diabetes. However, since the effectiveness of medical treatment of diabetes for patients at older ages (above 50 years) remains controversial, the deaths of individuals aged 50 years and above due to diabetes are not included in the amenable mortality figures.
The list of diseases and conditions and age groups to calculate amenable and preventable deaths was approved by the Members of Eurostat's Working Group of Public Health Statistics. However, both the list of diseases and conditions, as well as the age limits, reflect current health expectations, medical technology and knowledge, and developments in healthcare public policy, and hence might be subject to change in the future.
The second step in the calculation amenable and preventable deaths is the summation of all deaths (within the age limits) where the underlying cause of deaths was included in the list of diseases and conditions for amenable and preventable deaths (as defined here). The underlying data used to calculate amenable and preventable mortality indicators is the causes of death data, which includes detailed information on the underlying cause of death of the deceased.[6] The data for causes of death is an annual data collection with a legal basis requiring all European Member States to send complete data to Eurostat.
Note that some diseases and conditions are included in both amenable and preventable death, since certain conditions are considered as both treatable and preventable. An example would be deaths due to ischaemic heart diseases, which might be successfully avoided through timely and effective health care (e.g. through thrombolytic therapy) and simultaneously through effective public health intervention to reduce the underlying risk factors (e.g. high blood pressure or reduced salt intake).
Annual data on amenable and preventable deaths are provided in absolute numbers and as standardised death rates.[7] Since most causes of death vary significantly by age and according to sex, the use of standardised death rates improves comparability over time and between countries as death rates can be measured independently of a population’s age structure.
Context
Assessing the performance of health care systems is of increasing importance in the EU. While amenable and preventable mortality indicators are not meant to be a definite measurement of the quality of the health care in Member States, they provide some indication for the quality and performance of health care and (wider) public health policies in a country. In addition to health care and public health policies, other factors related to the likelihood of individuals to contract a disease or to seek medical advice - such as education, social class, health beliefs, levels of concerns, costs of diagnosis and treatment - are likely to influence the amount of amenable and preventable deaths in countries.[8] Improvements in health policies should translate into lower values for amenable and preventable deaths. However, there is likely to be a long time lag between implementation of health (care) policies and changes in the mortality rates, and hence conclusions need to be drawn with caution.
See also
- Health in the European Union – facts and figures
- Causes of death statistics
- Cardiovascular diseases statistics
- Cancer statistics
- Specific cancers
- Respiratory diseases statistics
Further Eurostat information
Publications
- 1 in 4 deaths caused by cancer in the EU28 - Lung cancer main fatal cancer
- Causes of death in the EU - Issue number 10/2006
- Circulatory diseases - Main causes of death for persons aged 65 and more in Europe, 2009
Main tables
Database
Dedicated section
Methodology / Metadata
Source data for tables and figures (MS Excel)
External links
- European Commission, Directorate General Health and Food Safety — Mortality
- European Commission, Directorate General Health and Food Safety — Major and chronic diseases
- European Commission, Directorate General Health and Food Safety — Health systems performance assessment
Notes
- ↑ See the discussions in Nolte E. and M. McKee (2004): "Does Health Care Save Lives? Avoidable Mortality Revisited", Nuffield Trust, London, 1-93; and Gay et al. (2011): "Mortality Amenable to Health Care in 31 OECD Countries". OECD Health Working Papers No. 55, OECD.
- ↑ See page 18 of Nolte E. and M. McKee (2004), "Does Health Care Save Lives? Avoidable Mortality Revisited", Nuffield Trust, London
- ↑ Avoidable deaths are all deaths that are defined as preventable, amenable or both, and where each death is counted only once. Note that some diseases and conditions are included in both amenable and preventable death, since certain conditions are considered as both treatable and preventable. An example would be deaths due to ischaemic heart diseases, which might be successfully avoided through timely and effective health care (e.g. through thrombolytic therapy) and simultaneously through effective public health intervention to reduce the underlying risk factors (e.g. high blood pressure or reduced salt intake).
- ↑ Note that the total number of avoidable deaths does not equal the sum of amenable and preventable. See note in Table 2.
- ↑ See definition from the Office for National Statistics (ONS), UK, 2011
- ↑ The causes of death data collection is documented in more detail in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
- ↑ Standardised deaths rates use the European Standard Population
- ↑ See page 18 of Nolte E. and M. McKee (2004), "Does Health Care Save Lives? Avoidable Mortality Revisited", Nuffield Trust, London