SDG 3 - Good Health and well-being
Ensure healthy lives and promote well-being for all at all ages
Data extracted in April 2024.
Planned article update: June 2025.
Highlights
This article is a part of a set of statistical articles, which are based on the Eurostat publication ’Sustainable development in the European Union — Monitoring report on progress towards the SDGs in an EU context — 2024 edition’. This report is the eighth edition of Eurostat’s series of monitoring reports on sustainable development, which provide a quantitative assessment of progress of the EU towards the SDGs in an EU context.
SDG 3 aims to ensure health and promote well-being for all at all ages by improving reproductive, maternal and child health; ending epidemics of major communicable diseases; and reducing non-communicable and mental diseases. It also calls for reducing behavioural and environmental health risk factors.
Full article
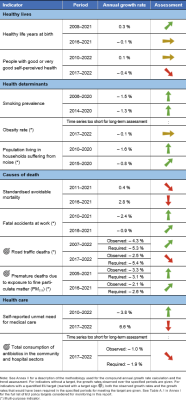
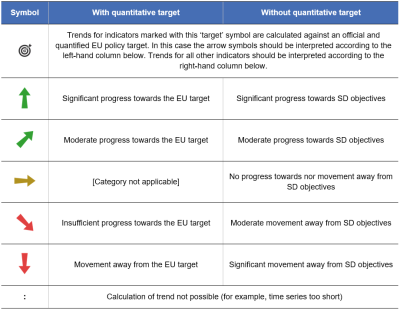
Good health and well-being in the EU: overview and key trends
Health can be defined as ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’ [1]. Good health is not only of value to the individual as a major determinant of quality of life, well-being and social participation, it is also a basic precondition for general economic growth. Monitoring SDG 3 in an EU context focuses on the topics of healthy lives, determinants of health, causes of death and health care. Over the five-year period assessed, the EU experienced setbacks in around half of the indicators analysed here, leading to an overall slightly negative assessment of the goal as a whole. Some of the negative trends observed are related to the effects of the COVID-19 pandemic, which are only now becoming visible in the data. The most prominent of these trends include declines in healthy life expectancy, in self-perceived health and in unmet needs for medical care as well as an increase in the number of people dying from avoidable (preventable) causes. Developments have been more favourable in other indicators on health determinants and causes of death, even though the EU is currently not on track to meet some of its respective 2030 targets.
Healthy Lives
The worldwide surge in life expectancy over the past century is a result of various factors, including reduced infant mortality, rising living standards, improved lifestyles and better education, as well as advances in health care and medicine.
While life expectancy has increased in EU countries over the past few decades, the pace of progress has slowed in recent years in many of those countries. The COVID‑19 pandemic resulted in a decline in life expectancy in most EU countries in 2020 and 2021, followed by a moderate recovery in 2022 [2]. However, while life expectancy gives an objective assessment of how long people can expect to live, it does not show whether people live their lives in good health. Thus, two indicators are now included in the analysis. The first one, healthy life years at birth, shows the number of years a person can expect to live in a healthy state. The second one measures the share of people with good or very good perceived health, capturing an individual’s subjective view of their well-being.
The COVID-19 pandemic has reduced the healthy life expectancy and self-perceived health of the EU population
In 2021, a child born in the EU could on average expect to live 63.6 years without any severe or moderate health problems. This is 1.0 years lower than at the pre-pandemic peak of 64.6 years in 2019. While healthy life expectancy had increased between 2016 and 2019, it fell in 2020 and 2021 due to the impact of the COVID-19 pandemic. Overall, the 2021 value is 0.4 years lower than the 64.0 years recorded in 2016. However, the overall EU figure masks considerable differences within and between Member States, with healthy life expectancy varying by 14.9 years between countries in 2021. This difference is narrower than in 2020, when it amounted to 19.3 years.
The impact of the pandemic is also reflected in the data for self-perceived health. While the proportion of EU citizens rating their own health as good or very good increased between 2017 and 2020, it fell again in 2021 and 2022, reaching 67.8 % in 2022. This is 1.2 percentage points lower than in 2017. Similar to healthy life expectancy, this share varied strongly across Member States, ranging from 48.1 % in Lithuania to 80.1 % in Ireland. Furthermore, differences also exist between rural and urban areas. In 2022, the percentage of people who perceived their health to be good or very good was highest in cities (69.6 %), slightly below the average in towns and suburbs (67.5 %) and lowest in rural areas (65.4 %) [3]. Moreover, the share of people with a disability — capturing a long-standing limitation to perform usual activities — who perceived their health as being good or very good was significantly lower than the EU average. Only 26.8 % of people with a moderate disability and even only 7.3 % of people with severe disability perceived their health as being good or very good in 2022, while 84.7 % of people without a disability did so [4].
Women have a higher healthy life expectancy than men, but are less likely to assess their health as being good
Between 2016 and 2021, the number of healthy life years that women could expect at birth decreased by 0.2 years, from 64.4 years to 64.2 years. During the same period, the healthy life years men could expect at birth fell by 0.5 years — from 63.6 in 2016 to 63.1 years. Thus, women were not only associated with a higher absolute number of healthy life years, their healthy life expectancy also fell more slowly than it did for men. The gap between the two examined sexes consequently rose from 0.8 years in 2016 to 1.1 years in 2021. In the same year, in about three out of four Member States, women could expect a higher number of healthy life years at birth than men.
Despite their higher healthy life expectancy at birth, women were less likely than men to rate their health as good or very good: 65.4 % of women and 70.3 % of men perceived their health as being good or very good in 2022 — a gap of 4.9 percentage points.
Excess mortality fell and life expectancy improved in the EU in 2022
The COVID-19 pandemic considerably affected death rates in EU Member States throughout 2020 and 2021 [5]. The population above the age of 60 years, as well as people from socially disadvantaged groups, were especially affected [6]. Overall, between January 2020 and February 2023, about 1.74 million excess deaths were recorded in the EU and European Free Trade Association (EFTA) countries compared with the average number of deaths registered during the period 2016 to 2019. In February 2023, for the first time since February 2020 (pre-COVID-19 pandemic period), there were no excess deaths and the indicator fell below the baseline to – 1.1 %. In March and April 2023, excess mortality rose slightly to 1.3 % and 4.2 % respectively. In May 2023, when the World Health Organization declared an end to the COVID-19 public-health emergency, the excess mortality in the EU was 3.6 % [7].
The decrease in life expectancy across the EU caused by the COVID-19 pandemic appears to have halted in 2022. While life expectancy at birth fell in 2020 and 2021 compared with the previous year, it increased by 0.6 years in 2022. Nevertheless, with 80.7 years in 2022, it remained 0.6 years below the pre-pandemic value of 81.3 years reported in 2019 [8].
Health Determinants
Many factors affect the health of individuals and populations. These include socio-economic factors, the state of the environment, city design, access to and use of health services, and individual characteristics and behaviour [9]. Lifestyle-related risk factors, such as an unhealthy diet, physical inactivity, smoking and excessive alcohol consumption, directly affect citizens’ quality of life and life expectancy. These factors also have a negative impact on the health and social systems of EU Member States, government budgets, and economic productivity and growth. The health determinants discussed in the following sections are obesity rate , smoking prevalence and noise pollution. In addition, further factors such as mobility and consumption patterns may also influence the health determinants described below.
More than half of the adult EU population was overweight in 2022
Obesity is a serious public health problem because it significantly increases the risk of chronic diseases, such as cardiovascular disease, type-2 diabetes, hypertension and certain types of cancer. For some individuals, obesity may also be linked to a wide range of psychological problems. From a societal perspective, obesity has substantial direct and indirect costs that put a considerable strain on health and social security systems. Furthermore, being obese or overweight from an early age can lead to more health problems in the long term [10].
In 2022, 14.8 % of the EU population aged 18 or above were obese (with a body mass index equal to or greater than 30) and another 36.5 % were pre-obese (with a body mass index between 25 and 30) [11]. In total, more than half of the EU population aged 18 or above were obese or pre-obese (and therefore overweight). Between 2017 and 2022, the share of both obese and pre-obese people decreased slightly by 0.1 and 0.4 percentage points, respectively. The total share of overweight people thus decreased slightly over this period, from 51.8 % in 2017 to 51.3 % in 2022.
The obesity rate generally increases with age, peaking at age group 65 to 74 years (19.7 % obese in 2022) and decreasing again for people aged 75 and older. Young people aged 25 to 34 showed the lowest obesity rates, at 9.7 % in 2022. Moreover, obesity and pre-obesity rates decrease with higher educational levels, with 2022 obesity rates ranging from 10.5 % for people with tertiary education to 17.9 % for people with lower secondary education or lower [12]. In 2022, there was furthermore a considerable difference between Member States, with values ranging from 7.1 % in Italy to 26.1 % in Malta for obese people aged 18 and over.
Smoking prevalence among people aged 15 and over has decreased since 2006
Tobacco consumption is considered the single most preventable cause of illness and death worldwide. The World Health Organisation’s (WHO) European Region — that also includes some non-European countries such as Israel, and some in Central Asia [13] — has one of the highest mortality rates attributable to tobacco use [14]. Tobacco use is currently the leading cause of 16 % of all deaths among adults aged 30 years and over in Europe, which is above the global average of 12 %. Many of these premature deaths result from multiple types of cancer and cardiovascular and respiratory diseases linked to tobacco use [15].
Smoking prevalence among the population aged 15 or over fell between 2006 and 2020, from 31 % to 25 %. In 2020, more men (28 %) than women (22 %) reported that they smoke. However, the decline in smoking prevalence is less evident for women than for men, which can partially explain the narrowing gap in life expectancy between the sexes [16]. The age group with the highest prevalence of smokers were those aged 25 to 54 (close to 30 %) followed by younger respondents aged 15 to 24 (20 %) and older people aged 55 years and above (18 %). Lastly, the share of smokers who indicated having trouble paying bills most of the time is higher than the share of smokers who said they (almost) never have trouble paying bills [17].
The number of people affected by noise from neighbours and the street has slightly decreased in the EU
Noise exposure reduces life satisfaction and perceived well-being. In addition, transport noise has been identified as the second most significant environmental cause of ill health in western Europe after air pollution [18]. The most harmful health problems — such as those affecting the cardiometabolic system — arise because of interrelated issues including decreased sleep quality and stress reactions in the human body. These issues can also lead to premature death [19]. In Europe, environmental noise is estimated to contribute to 12 000 premature deaths per year [20]. Road traffic is the dominant source of environmental noise, but railways, airports and industry also remain important sources of localised noise pollution [21]. The WHO Environmental Noise Guidelines for the European Region provide recommendations for protecting human health from exposure to environmental noise that originates from various sources.
In this publication, the perception of noise pollution is measured by the share of the population living in households who report they suffer from noise from neighbours or the street. Since this measure is derived from subjective questions, a fall in the value of this indicator does not necessarily indicate a similar reduction in actual noise-pollution health effects that are instead calculated based on large-scale assessments and precise formulas derived by the WHO [22]. Over the past decade, the share of the EU population feeling affected by noise from neighbours or the street fell from 20.6 % in 2010 to 17.6 % in 2020. The perception of noise pollution is also unevenly distributed between Member States. In 2020, the proportion of people reporting noise disturbance from neighbours or the street ranged from 8.0 % in Estonia to 30.8 % in Malta.
Causes of Death
Causes of death are among the oldest medical statistics available and play a key role in the general assessment of health in the EU. The data can be used to determine which preventive and medical curative measures or investment in research might increase a population’s life expectancy. The indicators selected for this sub-theme look at avoidable mortality, air pollution and fatal accidents on roads and at work.
The COVID-19 pandemic seems to have led to more avoidable deaths
Avoidable mortality refers to preventable and treatable causes of death, including injuries and drug-related diseases, as well as respiratory and infectious diseases, and some types of cancer. While avoidable mortality had been decreasing until 2019, the COVID-19 pandemic appears to have reversed the trend. Between 2016 and 2021, preventable mortality rose by 23.6 %, from 162.5 per 100 000 persons in 2016 to 200.8 per 100 000 in 2021. This result may be a consequence of the COVID-19 pandemic: health systems operated close to their capacity limits in many EU countries, which might have prevented health care professionals from providing patients with the health care they needed on time, or even at all. On the other hand, treatable mortality increased only marginally by 0.1 %, from 93.2 per 100 000 persons to 93.3 in 100 000, over the same period. In total, avoidable mortality increased by 15.1 % in the EU, from 255.6 per 100 000 persons in 2016 to 294.1 per 100 000 persons in 2021. While the developments were nevertheless positive in many Member States, the gap of 517.3 persons per 100 000 in 2021 between the highest (694.8 in Romania) and the lowest (177.5 in Sweden) value shows there remains a great deal of variability within the EU.
The number of premature deaths due to exposure to air pollution by fine particulate matter in the EU has fallen
According to the WHO, air pollution is the number-one environmental cause of death in Europe [23]. It can lead to or aggravate many chronic and acute respiratory and cardiovascular diseases. Air pollution has been one of the EU’s main environmental policy concerns since the late 1970s. Air pollutants are emitted both naturally and as a result of human activities, with important sources being solid fuel combustion for domestic heating, industrial activities, road transport and agriculture. Urban populations are particularly exposed because of the daily flow of commuters, and the high concentration of industry and human activities causing the emission of fine particulate matter in EU cities. In addition, the most vulnerable citizens remain disproportionately affected by air pollution [24]. For example, groups with lower socioeconomic status tend to be disproportionately affected by air pollution because they often live closest to its source. Children are another disproportionally affected group because they have higher respiratory rates than adults, which increases their exposure to air pollution. Also, children’s developing immune systems and organs make them more vulnerable to air pollution [25]. Air pollution also has a significant negative impact on the economy, by reducing both productivity and life expectancy, as well as by increasing health costs [26].
Fine particulate matter (PM2.5) is one of the most harmful components of air pollution for human health, causing 253 305 premature deaths in Europe in 2021. Between 2005 and 2021, premature deaths due to exposure to PM2.5 decreased by 41 %. This development suggests the EU is on track to meeting its target of reducing the negative impact of air pollution on health by 55 % by 2030 compared with 2005, as set out in the Zero Pollution Action Plan (see ‘Zero pollution’ monitoring and outlook). According to an analysis by the European Environment Agency (EEA), if the trend seen in the past ten years were to continue, the decline in the premature mortality attributable to PM2.5 would reach 68 % by 2030 relative to 2005 levels.
Fatal work and road accidents have decreased, but further progress is necessary to meet the 2030 target of halving deaths from road crashes
Accidents were one of the most common causes of death within the EU in 2021, leading to more than 165 000 deaths or 3.1 % of all deaths [27]. These accidents may happen at different places such as at home, leisure venues or work, as well as while travelling. Improving the working environment to protect employee health and safety is an important objective set out by the EU and its Member States in the Treaty on the Functioning of the European Union. Halving the number of deaths from road-traffic crashes is not only a global target, but also a goal of EU policies. The EU road safety policy framework 2021–2030 sets a target of reducing deaths and serious injuries by 50 % by 2030 compared with 2019.
In 2022, 20 653 people were killed in road traffic crashes, equalling 4.6 per 100 000 people. This represents a 11.7 % reduction compared with 2017, due in part to lower traffic volumes during the COVID-19 pandemic. However, the number of road fatalities has grown by 9.7 % since its 2020 low, and the EU is consequently not on track to meet the target of halving the number of people killed in road traffic crashes by 2030 compared with 2019 levels. Nevertheless, the EU rate of 4.6 fatalities per 100 000 people compares favourably with the global average of around 15 per 100 000 [28]. Preliminary results for 2023 indicate that fatalities remained below the pre-pandemic level: in 2023 road deaths fell slightly by 1 % compared with 2022 and remained 10 % lower than before the pandemic in 2019 [29]. For further details see the article on SDG 11 ‘Sustainable cities and communities’.
Fatal accidents, leading to a person’s death within one year, may also occur at work. The EU made progress on this indicator between 2016 and 2021, reducing the number of fatal accidents at work per 100 000 employed persons from 1.84 to 1.76. There is a considerable difference between the sexes: the incidence rate for women (0.26) was negligible compared with the rate for men (3.08). This difference can be explained by the higher share of men working in professions associated with a higher risk of work accidents. Non-fatal accidents can also cause considerable harm, for example by leading to a permanent disability that may force people to leave the labour market or change their job. Non-fatal accidents happened considerably more often than fatal accidents, with an incidence rate of 1 516 per 100 000 employed persons in 2021 [30].
Health Care
Access to health care — the timely access to affordable, preventive and curative health care — is high on the political agenda of most EU countries. It is defined as a right in the Charter of Fundamental Rights and is one of the 20 principles of the European Pillar of Social Rights. Limited access for some population groups, especially vulnerable populations, people with disabilities, transgender and intersex people, may result in poorer health outcomes and greater health inequalities. Reducing health inequalities is not only important for equity reasons, but also because it contributes to higher economic and social cohesion [31].
Unmet needs for medical care have increased since 2017
In 2022, 2.2 % of the EU population reported an unmet need for medical care because of financial reasons, long waiting lists or travel distance. This represents a 0.6 percentage point increase since 2017, when the share was 1.6 %. Differences between Member States’ reported unmet needs for medical care remained substantial, amounting to 9 percentage points in 2022. While in Cyprus 0.1 % of the population reported an unmet need for medical care in 2022 for the reasons monitored, around 9 % of the population did so in Greece and Estonia.
Financial constraints are the most common reason why people report unmet needs for medical examination. On average, for 1.1 % of the total EU population in 2022, ‘too expensive’ was the most prominent reason for reporting unmet medical examination. Furthermore, financial constraints were the most common self-reported reason for unmet needs in rural areas (1.3 %), which was slightly more than for people in towns or suburbs and in cities (1.1 % each). A further 0.9 % across all degrees of urbanisation reported ‘waiting lists’ as a reason for unmet needs for medical examination. This reason for unmet medical needs was more often declared in cities (1.1 %) than in rural areas (0.9 %) and in towns and suburbs (0.8 %). Another 0.1 % described ‘too far to travel’ as the main reason for an unmet need for medical examination. This was more often the case in rural areas (0.2 %) than in cities, or in towns and suburbs (both 0.1 %). However, not all Member States listed cost as the main reason for unmet needs — in many countries waiting lists were cited by most people [32].
Moreover, people with disabilities find it more difficult to access health care. In 2022, 6.3 % of people with severe activity limitations and 4.2 % of people with some activity limitations reported unmet needs for medical care due to the monitored reasons (financial, waiting list or distance), compared with only 1.2 % of people without disabilities [33]. This discrepancy indicates that access to health care remains a challenge not only in certain parts of the EU but also for certain population groups.
Most European countries have achieved universal coverage for a core set of services, which usually include consultations with doctors, tests, examinations and hospital care. Yet in some countries, coverage of these services may not be universal or patients may have to bear the costs of accessing them. Furthermore, across the EU, around a seventh of all health spending was borne directly by households in 2020. Out-of-pocket payments as a share of total current health expenditure decreased slightly from 15.9 % in 2014 to 14.5 % in 2021. However, a considerable gap of 25.1 percentage points between countries remained in 2021 [34]. Such out-of-pocket payments can pose a serious problem for low-income households, in particular if combined with reduced financial resources for the health care system caused, for example, by an economic crisis [35]. Moreover, across Member States, between 1.0 % and 19.2 % of households experienced catastrophic spending on health, meaning out-of-pocket spending on health care exceeded 40 % of a household’s disposable income [36]. Poor households and those who have to pay for long-term treatment such as medicines for chronic illness are at high risk of experiencing financial hardship as a result of having to pay out of their own pockets.
Specific population groups may not have the same access to health services as the general population
In many EU countries minorities do not have the same access to health services as the general population. One of those minorities is the Roma people. According to a study based on survey data from 2021 the share of Roma people who experienced discrimination in terms of access to health services increased between 2016 and 2021 in most of the 13 EU and non-EU countries examined by the Fundamental Rights Agency. The same survey provides evidence that women were more often discriminated against than men. Furthermore, the youngest and the oldest respondents reported lower levels of discrimination compared with middle-aged respondents: the age group 16 to 24 experienced discrimination in 10 % of cases, while respondents aged 65 and above reported discrimination in 13 % of cases. At the same time, 16 % of respondents aged 25 to 64 reported they had experienced discrimination. In terms of health outcomes, the study also found that Roma people have a markedly lower life expectancy (by 11.0 years for women and 9.1 years for men) than the general population in the EU.
People of African descent are more likely to report having unmet medical needs in most EU Member States according to a study of the Fundamental Rights Agency, based on survey data collected in 15 EU Member States in 2022. Overall, around every 10th respondent (9 %) reported that they had an unmet need for a medical examination or treatment in the year before the survey. This is nearly two times the rate of the general population in the EU (5 %). Further, every 10th respondent of African descent (9 %) felt racially discriminated against in the 12 months before the survey when accessing healthcare services. Considerable differences among Member States were observed. The highest 12-month prevalence of racial discrimination in access to healthcare was reported by respondents in Austria (28 %), Germany (27 %) and Finland (18 %). The lowest rates reported were from France, Poland and Portugal (5 % each).
The 2nd LGBTI Survey, conducted by the Fundamental Rights Agency in 2019, found that 16 % of LGBTI people felt discriminated when in contact with healthcare or social services staff. Notably, 52 % of respondents who assessed their general health as ‘very bad’ and 36 % of those who assessed it as ‘bad’ felt discriminated against in healthcare settings. Perceived discrimination was lower among those who assessed their health as ‘very good’ or ‘good’ (1 % and 14 %, respectively).
The total consumption of antibiotics in the EU has fallen, although there are substantial differences between Member States
Antimicrobial resistance (AMR) is a serious cross-border threat to health in the EU [37]. From 2016 to 2020, AMR led to more than 35 000 deaths in the EU/EEA each year [38]. Policies that tackle AMR with a ‘One-Health’ approach can save lives and healthcare costs. Antimicrobial consumption (AMC) is one of the main drivers of the development of AMR. This is aggravated by the inappropriate use of antimicrobials in humans, animals and plants. Reduction of AMC by using antimicrobials prudently and only where needed reduces selective pressures on the pathogens that contribute to the development of multi-drug resistance.
In humans, AMC is expressed as the number of defined daily doses (DDD) per 1 000 inhabitants per day, providing an estimate of the proportion of the population treated daily with antimicrobials. The 2022 EU population-weighted mean total AMC in the community and hospital sectors of antibacterials for systemic use (ATC group J01) was 19.4 DDD per 1 000 inhabitants per day. A statistically significant decrease was observed for the EU population-weighted mean consumption between 2013 and 2022 [39]. In the short term, the EU population-weighted mean total consumption of antibacterials for systemic use has decreased by 4.9 % since 2017, indicating only slow progress towards the EU target of reducing the total consumption of antibiotics in humans by 20 % by 2030 relative to 2019 [40]. Additionally, significant differences between Member States can be observed. In 2022, country-specific means ranged from 9.1 DDD per 1 000 inhabitants per day in the Netherlands to 33.5 in Cyprus.
Antimicrobial-resistant bacteria derived from food-producing animals can spread to humans by ingestion of or from handling food contaminated with zoonotic bacteria. Over time, this makes the antimicrobials less effective, resulting in treatment failure [41]. Thus, in addition to reducing human consumption of antimicrobials in the community and hospital sectors, the EU has set a target, in its Farm to Fork Strategy, to reduce overall EU sales of antimicrobials for farmed animals and in aquaculture by 50 % by 2030 relative to 2018. According to a 2023 report from the European Medicines Agency (EMA), EU Member States have already attained more than half of the targeted reduction. In 2022, sales of veterinary antimicrobial agents amounted to 84.8 milligrams per population correction unit (mg/PCU), which is a 28.3 % decrease compared with the 2018 baseline of 118.3 mg/PCU. Nevertheless, despite this achievement, the EMA report notes that Member States will have to continue taking action in order to further reduce their overall aggregated sales of antimicrobials and reach the 2030 goal of 59.2 mg/PCU. Maintaining an annual decrease in sales of about 5 % over the remaining years would keep Member States on track to reach the 2030 target.
Main indicators
Healthy life years at birth
This indicator measures the number of years at birth that a person can expect to live in a healthy condition. Healthy life years is a health expectancy indicator which combines information on mortality and morbidity (prevalence of the population suffering from a disease or medical condition).
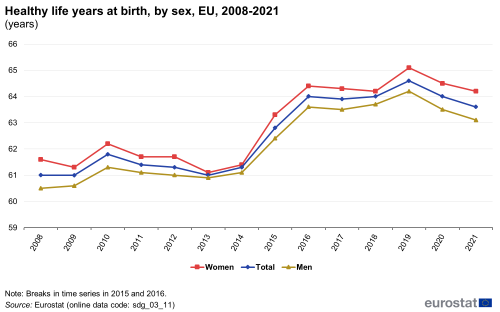
Note: y-axis does not start at 0.
Source: Eurostat (sdg_03_11)
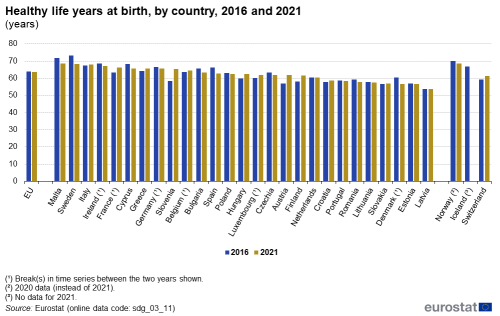
Source: Eurostat (sdg_03_11)
People with good or very good self-perceived health
This indicator is a subjective measure of how people judge their health in general on a scale from ‘very good’ to ‘very bad’. The data stem from the EU Statistics on Income and Living Conditions (EU-SILC). Indicators of perceived general health have been found to be a good predictor of people’s future health care use and mortality.
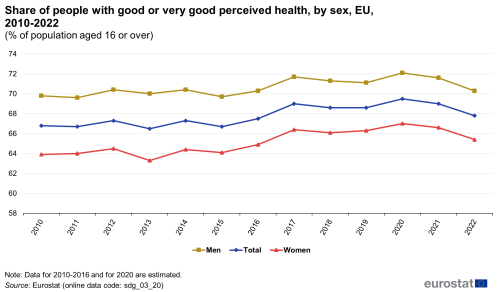
Note: y-axis does not start at 0.
Source: Eurostat (sdg_03_20)
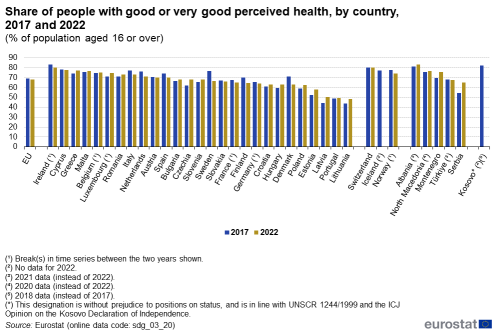
Source: Eurostat (sdg_03_20)
Smoking prevalence
This indicator measures the percentage of the population aged 15 years and over who report they currently smoke boxed cigarettes, cigars, cigarillos or a pipe. It does not include the use of other tobacco and related products such as electronic cigarettes and snuff. The data are collected through a Eurobarometer survey and are based on self-reported use during face-to-face interviews in people’s homes.
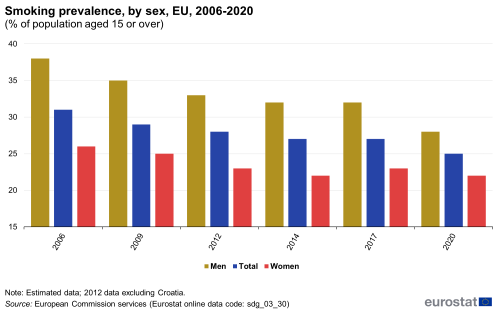
Note: y-axis does not start at 0.
Source: European Commission services, Eurostat (sdg_03_30)
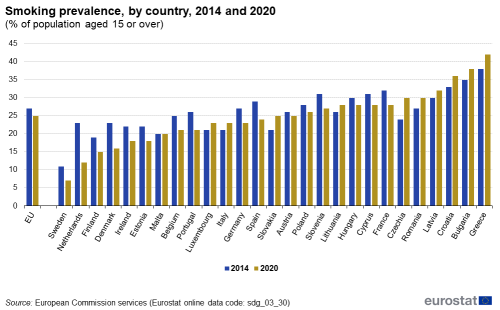
Source: European Commission services, Eurostat (sdg_03_30)
Standardised avoidable mortality
Avoidable mortality covers both preventable and treatable causes of mortality. Preventable mortality refers to mortality that can mainly be avoided through effective public health and primary prevention interventions (carried out before the onset of diseases/injuries to reduce incidence). Treatable mortality can mainly be avoided through timely and effective health care interventions, including secondary prevention and treatment (after the onset of diseases to reduce case-fatality). The total avoidable mortality rate includes a number of infectious diseases, several types of cancers, endocrine and metabolic diseases, as well as some diseases of the nervous, circulatory, respiratory, digestive and genitourinary systems, some diseases related to pregnancy, childbirth and the perinatal period, a number of congenital malformations, adverse effects of medical and surgical care, a list of injuries and alcohol and drug-related disorders.
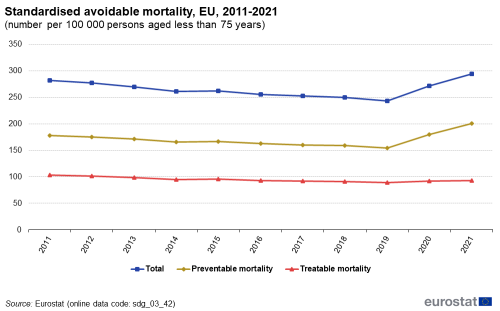
Source: Eurostat (sdg_03_42)
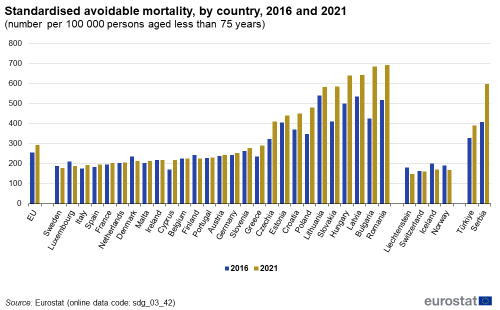
Source: Eurostat (sdg_03_42)
Self-reported unmet need for medical care
In the context of SDG monitoring, this indicator measures the share of the population aged 16 and over reporting unmet needs for medical care due to one of the following reasons: ‘financial reasons’, ‘waiting list’ and ‘too far to travel’. Self-reported unmet needs concern a person’s own assessment of whether they needed medical examination or treatment (dental care excluded) but did not have it or did not seek it. The data stem from the EU Statistics on Income and Living Conditions (EU-SILC). Since social norms and expectations may affect responses to questions about unmet care needs, caution is required when comparing differences in the reporting of unmet medical examination across countries. In addition, the different organisation of health care services is another factor to consider when analysing the data. Finally, there are also some variations in the survey questions across countries and across time [42].
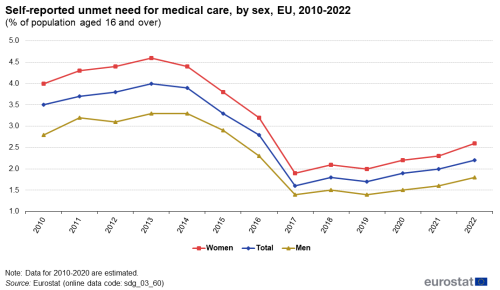
Note: y-axis does not start at 0.
Source: Eurostat (sdg_03_60)
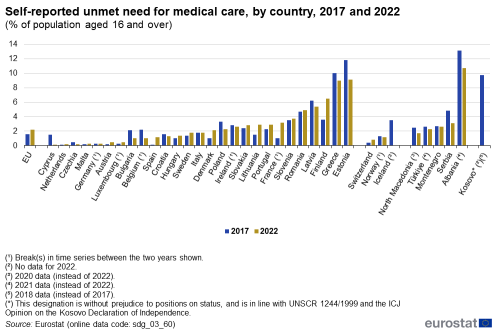
Source: Eurostat (sdg_03_60)
Total consumption of antibiotics in the community and hospital sectors
This indicator measures the total antimicrobial consumption (AMC) in the community and hospital sectors. AMC is expressed as the number of defined daily doses (DDD) per 1 000 inhabitants per day. The data refer to the Anatomical Therapeutic Chemical (ATC) classification code J01 ‘Antibacterials for systemic use’. The data for the EU aggregate are presented as population-weighted mean and include imputations and adjustments [43].
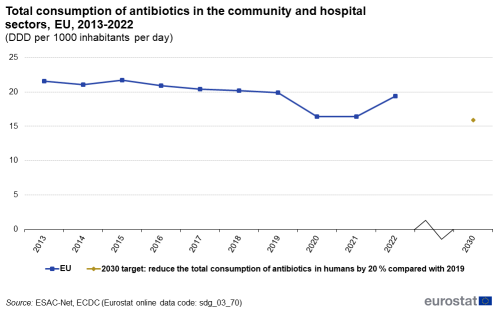
Source: Eurostat (sdg_03_70)
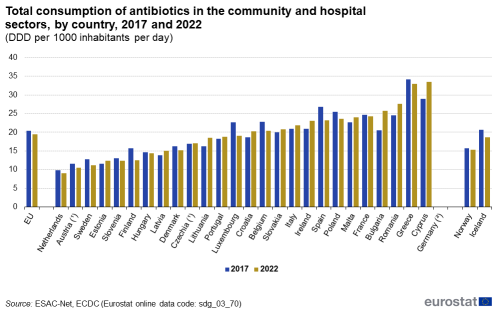
Source: Eurostat (sdg_03_70)
Direct access to
More detailed information on EU SDG indicators for monitoring of progress towards the UN Sustainable Development Goals (SDGs), such as indicator relevance, definitions, methodological notes, background and potential linkages can be found in the introduction as well as in Annex II of the publication ’Sustainable development in the European Union — Monitoring report on progress towards the SDGs in an EU context — 2024 edition’.
Further reading on good health and well-being
- EEA (2019), Healthy environment, healthy lives: how the environment influences health and well-being in Europe, European Environment Agency, Copenhagen.
- OECD & European Commission (2022), Health at a Glance: Europe 2022, OECD Publishing, Paris.
- WHO (2018), Environmental Noise Guidelines for the European Region, WHO Regional Office for Europe, Copenhagen.
- World Health Organization (2024), WHO report on the global tobacco epidemic, 2023: Protect people from tobacco smoke
Further data sources on good health and well-being
Notes
- ↑ World Health Organization (1946), Constitution of the World Health Organization.
- ↑ Source: Eurostat (online data code: (demo_mlexpec)).
- ↑ Source: Eurostat (online data code: (hlth_silc_18)).
- ↑ Source: Eurostat (online data code: (HLTH_DH010)).
- ↑ Eurostat (2023), Statistics Explained: Mortality and life expectancy statistics.
- ↑ OECD/EU (2020), Health at a Glance. Europe 2020 — State of Health in the EU Cycle, OECD Publishing, Paris, p. 12.
- ↑ Source: Eurostat (online data code: (demo_mexrt)).
- ↑ Source: Eurostat (online data code: (demo_mlexpec)).
- ↑ World Health Organization (2024), Social determinants of health.
- ↑ World Health Organization (2021), Obesity: New analysis from WHO/Europe identifies surprising trends in rates of overweight and obesity across the Region.
- ↑ The indicator measures the share of obese people based on their body mass index (BMI). BMI is defined as the weight in kilograms divided by the square of the height in metres. People aged 18 years or over are considered obese with a BMI equal to or greater than 30. Other categories are: underweight (BMI less than 18.5), normal weight (BMI between 18.5 and less than 25), and pre-obese (BMI between 25 and less than 30). The category overweight (BMI equal or greater than 25) combines the two categories pre-obese and obese.
- ↑ Source: Eurostat (online data code: (ilc_hch10)).
- ↑ The WHO European Region also includes some non-European countries such as Israel, Uzbekistan, Turkmenistan or Tajikistan; see https://www.who.int/countries for the full list of countries.
- ↑ World Health Organization (2012), WHO global report: mortality attributable to tobacco.
- ↑ World Health Organization (2024), WHO report on the global tobacco epidemic, 2023: Protect people from tobacco smoke.
- ↑ OECD/EU (2014), Health at a Glance: Europe 2014, OECD Publishing, Paris, pp. 16–17.
- ↑ European Commission (2021), Attitudes of Europeans towards tobacco and electronic cigarettes, Special Eurobarometer 506.
- ↑ European Environment Agency (2018), Environmental noise.
- ↑ European Environment Agency (2021), Managing exposure to noise in Europe.
- ↑ European Environment Agency (2020), Healthy environment, healthy lives: how the environment influences health and well-being in Europe, Publications Office of the European Union, Luxembourg.
- ↑ European Environment Agency (2021), Managing exposure to noise in Europe.
- ↑ Also see: European Environment Agency (2019), Environmental noise.
- ↑ European Environment Agency (2023), Briefing. Europe’s air quality status 2023.
- ↑ European Environment Agency (2018), Unequal exposure and unequal impacts: social vulnerability to air pollution, noise and extreme temperatures in Europe, Publications Office of the European Union, Luxembourg.
- ↑ Ibid.
- ↑ European Environment Agency (2022), Air quality in Europe 2022 and European Environment Agency (2024). Europe's air quality status 2024.
- ↑ Source: Eurostat (online data code: (hlth_cd_aro)).
- ↑ WHO (2023), Global status report on road safety 2023, Geneva.
- ↑ European Commission (2024), 2023 figures show stalling progress in reducing road fatalities in too many countries.
- ↑ Source: Eurostat (online data code: (hsw_mi08)).
- ↑ European Council (2014), Council conclusions on the economic crisis and healthcare, 2014/C 217/02.
- ↑ Source: Eurostat (online data code: (HLTH_SILC_21)).
- ↑ Source: Eurostat (online data code: (hlth_dh030)).
- ↑ Source: Eurostat (online data code: (HLTH_SHA11_HF)).
- ↑ Expert Panel on effective ways of investing in health (EXPH) (2016), Access to health services in the European Union, final opinion approved at the 14th plenary meeting of 3 May 2016 after public consultation, p. 18.
- ↑ OECD/EU (2020), Health at a Glance. Europe 2020 — State of Health in the EU Cycle, OECD Publishing, Paris, p. 207. Data refer to different years for the Member States, ranging from 2011 to 2018.
- ↑ European Parliament and the Council of the European Union (2022), Regulation 2022/2371 on serious cross-border threats to health and repealing Decision No 1082/2013/EU.
- ↑ European Centre for Disease Prevention and Control (ECDC) (2022), Assessing the health burden of infections with antibiotic-resistant bacteria in the EU/EEA, 2016–2020, ECDC, Stockholm, pp. 4-7.
- ↑ European Centre for Disease Prevention and Control (ECDC) (2022), Antimicrobial consumption in the EU/EEA (ESAC-Net). Annual Epidemiological Report for 2022.
- ↑ Council of the European Union (2023), Council Recommendation on stepping up EU actions to combat antimicrobial resistance in a One Health approach, 2023/C 220/01.
- ↑ European Food Safety Authority (EFSA) and European Centre for Disease Prevention and Control (ECDC) (2023), The European Union Summary Report on Antimicrobial Resistance inzoonotic and indicator bacteria from humans, animals and food in 2020/2021. EFSA Journal 2023;21(3):7867.
- ↑ OECD/EU (2018), Health at a Glance: Europe 2018 — State of Health in the EU Cycle, OECD Publishing, Paris, p. 170.
- ↑ European Centre for Disease Prevention and Control (2023), Antimicrobial consumption in the EU/EEA (ESAC-Net) — Annual Epidemiological Report 2022, ECDC, Stockholm.