Archive:The EU in the world - health
Data extracted in January and February 2020.
Planned article update: May 2022.
Highlights
Lowest health expenditure per inhabitant in 2016 among G20 members was in India.
The gender gap in life expectancy at birth in 2017 was higher for Russia than for other G20 members.
Among G20 members, the lowest proportions of overweight people (including obese) in 2016 were in India, both for men and for women.
(years)
Source: Eurostat (demo_mlexpec) and the World Bank (World Development Indicators)
This article is part of a set of statistical articles based on Eurostat’s publication The EU in the world 2020. It focuses on public health issues such as healthcare expenditure, provision and resources, as well as various health determinants in the European Union (EU) and the 16 non-EU members of the Group of Twenty (G20). The article gives an insight into health in the EU in comparison with (most of) the major economies in the rest of the world, such as its counterparts in the so-called Triad — Japan and the United States — and the BRICS composed of Brazil, Russia, India, China and South Africa.
Full article
Expenditure on health
Among G20 members, India had the lowest health expenditure per inhabitant in 2016
Healthcare systems are organised and financed in different ways. Monetary and non-monetary statistics may be used to evaluate how a healthcare system aims to meet basic needs for healthcare, through measuring financial, human and technical resources. Public expenditure on healthcare is often funded through government financing (general taxation) or social security funds. Private expenditure on healthcare mainly comes from direct household payments (also known as out-of-pocket expenditure) and private health insurance.
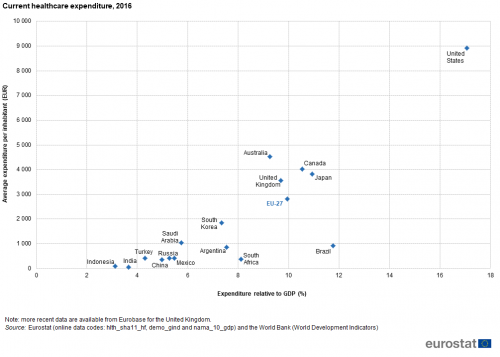
Among G20 members, the United States had by far the highest expenditure on health relative to gross domestic product (GDP), 17.1 % in 2016, almost double the 9.9 % recorded in the EU-27 (see Figure 1). Brazil, Japan and Canada each reported double-digit ratios in 2016. Spending on health in Turkey, India and Indonesia was less than 5.0 % of GDP.
Source: Eurostat (hlth_sha11_hf), (demo_gind) and (nama_10_gdp) and the World Bank (World Development Indicators)
Figure 1 also shows the absolute level of health expenditure per inhabitant in 2016. The information presented confirms the notably higher level of expenditure on health in the United States, where an average of EUR 8.9 thousand was spent per inhabitant. Expenditure in the range of EUR 3.6-4.5 thousand per inhabitant was recorded in Australia, Canada, Japan and the United Kingdom, followed by the EU-27 with average expenditure of EUR 2.8 thousand per inhabitant. By contrast, Indonesia and India recorded by far the lowest levels of health expenditure relative to population size among the G20 members, with averages of EUR 101 and EUR 57 per inhabitant respectively.
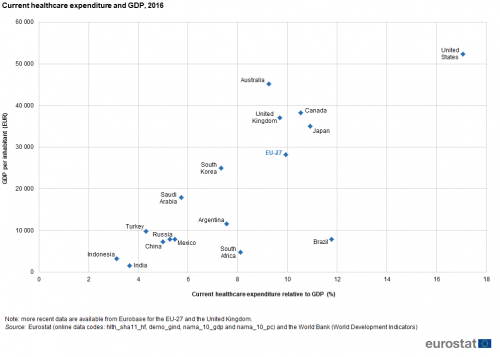
The different relative positions of the G20 members when comparing the two indicators shown in Figure 1 reflects differences in GDP per inhabitant. This is shown in Figure 2 where the ratio of expenditure on health relative to GDP is plotted against GDP per inhabitant. In general, G20 members with low levels of GDP per inhabitant in 2016 reported low ratios of healthcare expenditure relative to GDP, but there were exceptions. For example, Brazil reported a relatively high ratio of healthcare expenditure relative to GDP (11.8 %; second only to the United States), despite having the fifth lowest GDP per inhabitant. Equally, South Africa recorded a relatively high ratio of healthcare expenditure relative to GDP (8.1 %) given that it had the third lowest GDP per inhabitant.
Source: Eurostat (hlth_sha11_hf), (demo_gind), (nama_10_gdp) and (nama_10_pc) and the World Bank (World Development Indicators)
Life expectancy
The gender gap for life expectancy at birth in 2017 was notably higher in Russia than in other G20 members
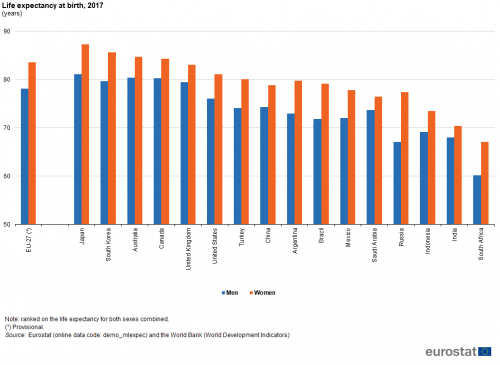
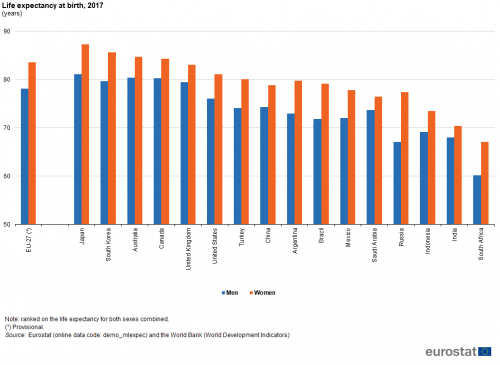
Among the G20 members, the highest life expectancy at birth in 2017 was recorded in Japan (84 years), while life expectancy was also above 80 years in South Korea, Australia, Canada, the United Kingdom and the EU-27. In two G20 members, life expectancy at birth in 2017 remained below 70 years: it stood at 69 years in India and 64 years in South Africa. The relatively low life expectancy for South Africa may be largely attributed to the impact of an HIV/AIDS epidemic: in 2018, 20 % of the population aged 15-49 years had the human immunodeficiency virus (HIV). In all G20 members, life expectancy was higher for females than for males (see Figure 3): this gender gap ranged from two years in India to seven years in Argentina, South Africa and Brazil, with a notably larger gap of 10 years in Russia.
(years)
Source: Eurostat (demo_mlexpec) and the World Bank (World Development Indicators)
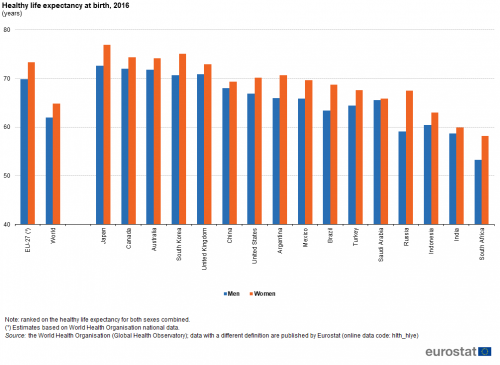
In line with the data for life expectancy, the highest expected number of healthy life years at birth among the G20 members in 2016 was in Japan (75 years), while in Canada, Australia, South Korea, the United Kingdom and the EU-27, the expected number of healthy life years for men and women combined was also higher than 70 years. In South Africa (56 years) and India (59 years), the expected number of healthy life years at birth in 2016 was notably lower than in other G20 members. The gender gap in terms of healthy life years was generally narrower than in terms of life expectancy, ranging with only one exception from almost no difference in Saudi Arabia to no more than five years in each of the remaining G20 members; in Russia the gap was eight years (see Figure 4).
Combining the data presented in Figures 3 and 4 indicates that, on average, people living in all G20 members could expect to live between 86 % and 90 % of their life free from disability (in other words, in a healthy state), with the lowest share recorded in Turkey and the highest in Mexico. In the EU-27, the share was 88 %.
Mortality
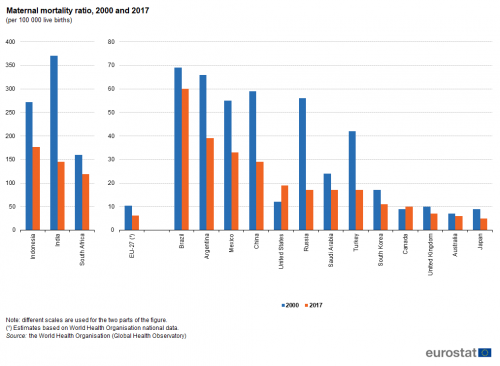
Almost all maternal deaths — those related to pregnancy and childbirth — occur in emerging and developing countries, with maternal mortality rates generally higher in their rural areas and among poorer communities. Most maternal deaths are preventable and according to the World Health Organisation the main causes are: severe bleeding (mostly bleeding after childbirth); infections (usually after childbirth); high blood pressure during pregnancy (pre-eclampsia and eclampsia); complications from delivery; and unsafe abortions.
The maternal mortality ratio shows the ratio between the number of maternal deaths and the number of live births, expressed per 100 000 live births (see Figure 5). While this ratio was relatively low in about half of the G20 members in 2017, it exceeded 100 per 100 000 live births in Indonesia (177), India (145) and South Africa (119), and was 60 per 100 000 live births in Brazil. The lowest ratios in 2017 — below 10 maternal deaths per 100 000 live births — were reported in the United Kingdom, the EU-27, Australia and Japan.
Between 2000 and 2017, the maternal mortality ratio fell in most G20 members, the exceptions being the United States, where the ratio increased considerably in relative terms (up by almost 60 %), and Canada, where an already low ratio rose slightly. Elsewhere, particularly large falls in the maternal mortality ratio were observed in India and Indonesia, as well as in South Africa, Russia, China, Argentina, Turkey and Mexico.
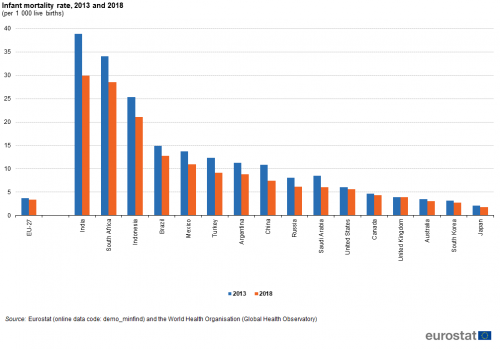
The infant mortality rate presents the ratio between the number of deaths of children aged less than one year and the number of live births in the same reference period; the resulting value is generally expressed per 1 000 live births. The progress made in medical healthcare services is reflected in the rapid decrease of infant mortality rates; indeed, all but one of the G20 members recorded falls in infant mortality rates between 2013 and 2018 (as shown in Figure 6), the exception being the United Kingdom where the rate was unchanged. The largest relative falls were recorded by China, Saudi Arabia and Turkey, where infant mortality rates fell by more than one quarter.
(per 1 000 live births)
Source: Eurostat (demo_minfind) and the World Health Organisation (Global Health Observatory)
The latest data available, for 2018, show that the lowest infant mortality rates among G20 members were recorded in Japan, South Korea, Australia, the EU-27, the United Kingdom and Canada, all under 5 deaths per 1 000 live births. By contrast, infant mortality rates in South Africa and India were more than six times as high, with rates of 29 and 30 deaths per 1 000 live births. Indonesia had the third highest infant mortality rate, while Brazil and Mexico were the only other G20 members to record double-digit rates in 2018.
Healthcare resources
The number of hospital beds per 100 000 inhabitants in the EU-27 in 2017 was the fourth highest among G20 members
Key indicators for measuring healthcare personnel are based on their number expressed per 100 000 inhabitants. With the notable exception of Argentina, there were more nurses and midwives than there were physicians in all of the G20 members. Relative to population size, the largest numbers of nurses and midwives in 2017 were recorded in Australia, the United States (data exclude midwives), Japan (2016 data) and Canada, all with at least 1 000 nurses and midwives per 100 000 inhabitants.
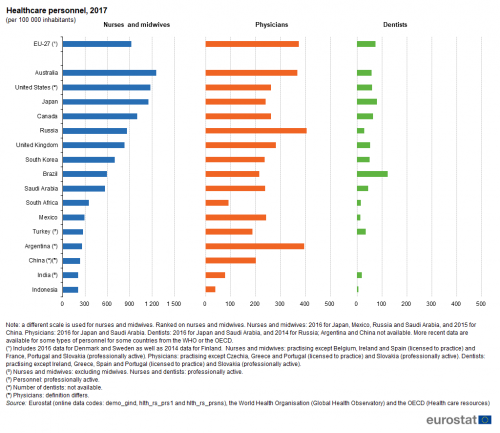
(per 100 000 inhabitants)
Source: Eurostat (demo_gind), (hlth_rs_prs1) and (hlth_rs_prsns), the World Health Organisation (Global Health Observatory) and the OECD (Health care resources)
The variation between the G20 members in the number of is the total number of physicians was relatively low in comparison with the other personnel indicators shown in Figure 7. The highest number of physicians relative to the overall population size in 2017 among the G20 members was recorded in Russia, followed closely by Argentina and then the EU-27 and Australia. At the other end of the range, South Africa, India and Indonesia recorded less than 100 physicians per 100 000 inhabitants; note that for India (as well as for China) the definition used differs.
Among the three indicators concerning healthcare personnel, the number of dentists per 100 000 inhabitants showed the greatest variation among the G20 members when taking account of their relatively low overall number. For example, Indonesia recorded an average of 5 dentists per 100 000 inhabitants in 2017, while in Brazil there were 124 dentists per 100 000 inhabitants in the same year. The average for the EU-27 was 74 dentists per 100 000 inhabitants.
Non-medical health determinants
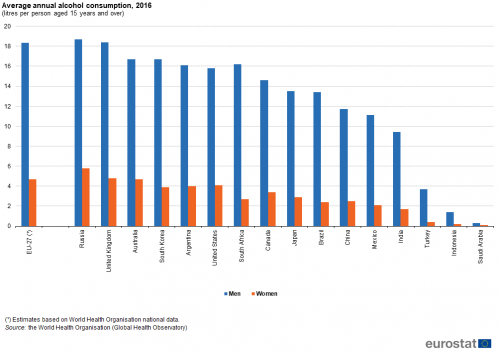
Figures 8 to 10 provide information on three non-medical health determinants, namely alcohol consumption, smoking and being overweight. The highest annual alcohol consumption in 2016 among G20 members was recorded for Russia (11.7 litres of alcohol per inhabitant aged 15 years and over), the United Kingdom (11.5 litres) and the EU-27 (11.3 litres). They were closely followed by Australia, South Korea, Argentina and the United States with annual alcohol consumption in the range of 9.8-10.6 litres per inhabitant. Relatively low average levels of alcohol consumption were recorded for India and Turkey, while the lowest levels were recorded in Indonesia (0.8 litres) and Saudi Arabia (0.2 litres); these low levels are influenced, to a large degree, by predominant religious beliefs in these countries. In all G20 members the average alcohol consumption in 2016 was greater among men than among women. In relative terms, the widest gender gap was recorded in Turkey where the average consumption by men was 9.3 times as high as that by women. The narrowest gender differences were recorded for Russia and Saudi Arabia where men on average men consumed about three times as much alcohol as women.
Indonesia reported the highest proportion of daily smokers: two fifths (40 %) of the population aged 15 years and over smoked in 2015. One quarter or more of the adult population in Russia (2016 data), Turkey (2016 data) and China (2015 data) smoked daily, while one fifth of the adult population smoked on a daily basis in the EU-27 (2014 data), and slightly less than one fifth in South Africa (2015 data), Japan, South Korea and the United Kingdom. Elsewhere, the incidence of daily smoking was at most 12 %, with a low of 8 % recorded in Mexico (note that the definition differs). In all G20 members the proportion of daily smokers in 2017 was greater among men than among women. The widest gender gap was recorded in Indonesia where 76 % of all men aged 15 years and over were daily smokers compared with just 4 % of women (2015 data). The narrowest gender differences were recorded for Canada, the United Kingdom, Australia (2016 data) and the United States.
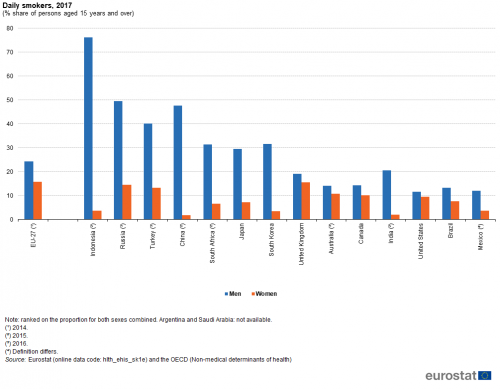
(% share of persons aged 15 years and over)
Source: Eurostat (hlth_ehis_sk1e) and the OECD (Non-medical determinants of health)
Among the G20 members, India recorded the lowest proportion of people being overweight in 2016, both for men and for women
The most frequently used measure for assessing whether someone is overweight (pre-obese or obese) is based on the body mass index (BMI), which evaluates weight in relation to height. According to the World Health Organisation, adults with a BMI above 25 are considered as overweight: those between 25 and 30 are considered as pre-obese and those with an index over 30 are considered obese.
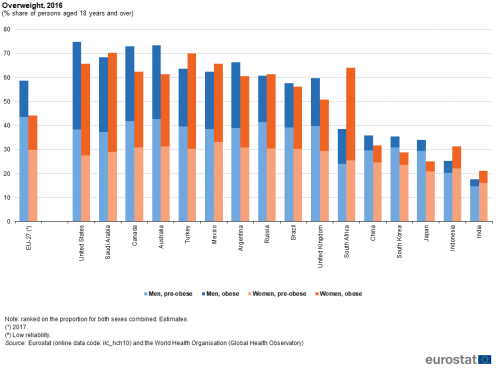
(% share of persons aged 18 years and over)
Source: Eurostat (ilc_hch10) and the World Health Organisation (Global Health Observatory)
The highest proportions of men that were overweight in 2016 were observed for the United States (75 % of the male population), Australia and Canada (both 73 %) — see Figure 10; note that the data presented may be based on measured results or self-reported data. By contrast, the highest proportions of overweight women were recorded in Saudi Arabia and Turkey (both 70 %), followed by the United States and Mexico (both 66 %). By contrast, a relatively low proportion of men were overweight in Indonesia (25 %) and India (18 %), while for women the lowest proportions were recorded in Japan (25 %) and India (21 %).
The proportion of overweight men was greater than the proportion of overweight women in a small majority of G20 members, with this gap between the sexes reaching more than 10 points in the EU-27, Australia and Canada. In the G20 members where the proportion of overweight women was higher than the proportion of overweight men, the differences were generally quite small, with the notable exception of South Africa where the gap was 25 points.
Among the G20 members there is far greater variability in the proportion of the population who were obese compared with the pre-obese proportion. Five Asian G20 members — China, India, Indonesia, Japan and South Korea — recorded particularly low proportions of their populations who were considered obese, less than 10 % for both men and for women. The share of obese men was smaller than the share of pre-obese men in all of the G20 members. Among women, this pattern was repeated in a majority of the G20 members, but not in Russia and Canada where the shares of pre-obese and obese women were nearly the same, nor in Turkey, the United States, Saudi Arabia and South Africa where the proportion of women who were obese was notably larger than the proportion that were pre-obese.
Source data for tables and graphs
Data sources
The statistical data in this article were extracted during January and February 2020.
The indicators are often compiled according to international — sometimes worldwide — standards. Although most data are based on international concepts and definitions there may be certain discrepancies in the methods used to compile the data.
EU data
Nearly all of the indicators presented for the EU and the United Kingdom have been drawn from Eurobase, Eurostat’s online database. Eurobase is updated regularly, so there may be differences between data appearing in this article and data that is subsequently downloaded. In some cases some data for the EU and for the United Kingdom have been extracted from international sources.
G20 members from the rest of the world
For the non-EU G20 members other than the United Kingdom, the data presented have mainly been compiled by the World Health Organisation; some data have been compiled by the OECD and some by the World Bank. For some of the indicators shown a range of international statistical sources are available, each with their own policies and practices concerning data management (for example, concerning data validation, correction of errors, estimation of missing data, and frequency of updating). In general, attempts have been made to use only one source for each indicator in order to provide a comparable dataset for G20 members.
Context
Health issues cut across a range of topics — including the provision of healthcare and protection from illness and accidents, such as consumer protection (food safety issues), workplace safety, environmental or social policies. The health statistics presented in this article address public health issues such as healthcare expenditure and resources, life expectancy and mortality, as well as a number of determinants of the health status of a population.
In many developed countries life expectancy at birth rose rapidly during the last century due to a number of factors, including reductions in infant mortality, rising living standards, improved lifestyles and better education, as well as advances in healthcare and medicine. Life expectancy at birth is one of the most commonly used indicators for analysing mortality and reflects the mean (additional) number of years that a person of a certain age can expect to live, if subjected throughout the rest of their life to the current mortality conditions.
Indicators of health expectancies, such as healthy life years (also called disability-free life expectancy) have been developed to study whether extra years of life gained through increased longevity are spent in good or bad health. These focus on the quality of life spent in a healthy state, rather than total life spans. Disability-free life expectancy is the number of years that a person is expected to continue to live in a healthy condition, in other words without limitation in functioning and without disability.
Direct access to
- The EU in the world 2020
- Statistics on European Neighbourhood Policy countries: South — 2020 edition
- The European Union and the African Union — A statistical portrait — 2019 edition;
- Key figures on the enlargement countries — 2019 edition
- Sustainable Development in the European Union — Monitoring report on progress towards the SDGs in an EU context
- Ageing Europe — 2019 edition
- Living conditions in Europe — 2018 edition
- Statistics on European Neighbourhood Policy countries: East — 2018 edition
- Globalisation patterns in EU trade and investment
- 40 years of EU-ASEAN cooperation — 2017 edition
- Asia-Europe Meeting (ASEM) — A statistical portrait — 2016 edition
- The European Union and the BRIC countries
- The European Union and the Republic of Korea — 2012
- Health (hlth), see:
- Health determinants (hlth_det)
- Tobacco consumption (hlth_smok)
- Smoking of tobacco products by sex, age and educational attainment level (hlth_ehis_sk1e)
- Tobacco consumption (hlth_smok)
- Health care (hlth_care)]
- Health care expenditure (SHA2011) (hlth_sha11)
- Health care expenditure — summary tables (hlth_sha11_sum)
- Health care expenditure by financing scheme (hlth_sh11a_hf)
- Health care expenditure — summary tables (hlth_sha11_sum)
- Health care resources (hlth_res)
- Health care staff (hlth_staff)
- Nursing and caring professionals (hlth_rs_prsns)
- Health personnel (excluding nursing and caring professionals) (hlth_rs_prs1)
- Health care staff (hlth_staff)
- Health care expenditure (SHA2011) (hlth_sha11)
- EU-SILC ad-hoc modules (ilc_ahm)
- 2017 - Health including children health (ilc_hch)
- Person distribution by body mass index, educational attainment level, sex and age (ilc_hch10)
- 2017 - Health including children health (ilc_hch)
- Population change - Demographic balance and crude rates at national level (demo_gind)]
- Mortality (demo_mor), see:
- Infant mortality rates (demo_minfind)
- Life expectancy by age and sex (demo_mlexpec)
- Main GDP aggregates (nama_10_ma)
- GDP and main components (output, expenditure and income) (nama_10_gdp)
- Auxiliary indicators (population, GDP per capita and productivity) (nama_10_aux)
- Main GDP aggregates per capita (nama_10_pc)
OECD
The World Bank
World Health Organisation (WHO)