Archive:Healthcare statistics
- Data from January 2014. Most recent data: Further Eurostat information, Main tables and Database. Planned article update: January 2015.

(% of current health expenditure) - Source: Eurostat (hlth_sha_hf)
(% of current health expenditure) - Source: Eurostat (hlth_sha_hc)

(% of current health expenditure) - Source: Eurostat (hlth_sha_hp)
(per 100 000 inhabitants) - Source: Eurostat (hlth_rs_prs), (tps00046) and (hlth_co_disch2t)
(per 100 000 inhabitants) - Source: Eurostat (tps00046)
(per 100 000 inhabitants) - Source: Eurostat (tps00168) and (tps00047)
(ISHMT - international shortlist for hospital morbidity tabulation), 2009
(per 100 000 inhabitants) - Source: Eurostat (hlth_co_disch2)

(ISHMT - international shortlist for hospital morbidity tabulation), average length of stay, 2009
(days) - Source: Eurostat (hlth_co_inpst)
This article presents key statistics on monetary and non-monetary aspects of healthcare in the European Union (EU). The state of health of individuals and of the population in general is influenced by genetic and environmental factors, cultural and socioeconomic conditions, as well as the healthcare services that are available to prevent and to treat illness and disease.
Healthcare systems are organised and financed in different ways across the EU Member States, but most Europeans would agree that universal access to good healthcare, at an affordable cost to both individuals and society at large, is a basic need.
Main statistical findings
Healthcare expenditure
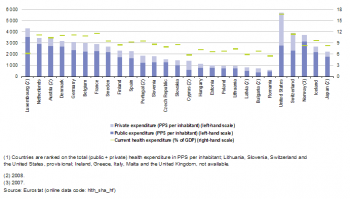
Total current healthcare expenditure (both in relative and absolute terms) varied significantly among the EU Member States in 2011 [1]. As shown in Figure 1, the share of current healthcare expenditure exceeded 10.0 % of gross domestic product (GDP) in six EU Member States (France, the Netherlands, Germany, Denmark, Belgium and Austria), which was almost double the share of current healthcare expenditure relative to GDP recorded in Cyprus, Estonia and Romania (all below 6.0 % of GDP).
The disparity was even bigger when comparing the level of total (public and private) healthcare spending per inhabitant, which varied from PPS 674 in Bulgaria to PPS 4 445 in Luxembourg. Notwithstanding the differences in organising and financing healthcare systems, these comparisons suggest that individuals living in those EU Member States with a higher average level of income per inhabitant generally spend more on purchasing healthcare goods and services.
Public and private healthcare expenditure by financing agent
The mix of public and private funding of healthcare in the EU reflects specific arrangements in healthcare financing systems. Table 1 provides an analysis of healthcare expenditure between public and private units that incur health expenditure. Public funding in the form of general government and social security funds dominates the healthcare sector in the majority of EU Member States, the main exception being Cyprus, where public funding accounted for a 42.1 % share of total healthcare expenditure. Aside from Cyprus and those EU Member States for which no data are available (Ireland, Greece, Croatia, Italy, Malta and the United Kingdom), the share of public funding in current healthcare spending ranged in 2011 from 56.2 % in Bulgaria to more than 80 % in Estonia, Sweden, Luxembourg, the Czech Republic, Denmark and the Netherlands.
An analysis of public financing of healthcare suggests that social security funds were a somewhat more popular means for funding healthcare within the EU Member States, as these accounted for three quarters or more of overall spending on healthcare in the Czech Republic (77.9 %) and the Netherlands (77.5 %) in 2011. By contrast, Denmark and Sweden reported that general government financing accounted for more than four fifths (84.6 % and 81.6 % respectively) of their total current expenditure on healthcare.
Private expenditure on healthcare is often used as an indicator to measure the accessibility of healthcare systems. The major source of private funding was direct household payments, referred to as out-of-pocket expenditure, which peaked in terms of its share of current healthcare expenditure in Cyprus (50.2 %) and Bulgaria (42.6 %), falling to a single-digit share in France and the Netherlands (7.7 % and 6.0 % respectively). Private insurance generally represented a small share of healthcare financing among the EU Member States for which data are available; its relative share only exceeded 10 % in France and Slovenia.
Healthcare expenditure by function
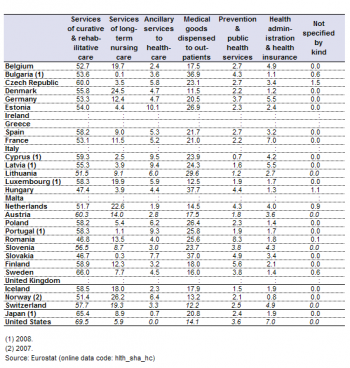
The functional patterns of healthcare expenditure presented in Table 2 show that in 2011 curative and rehabilitative services incurred more than 50.0 % of current healthcare expenditure in the majority of EU Member States for which data are available, the exceptions being Hungary, Slovakia and Romania.
Medical goods dispensed to outpatients was the second largest function, with average spending accounting for around one quarter of total current healthcare expenditure — although with a significant degree of variation, the lowest share of 11.5 % was recorded for Denmark, rising to more than one third of the total in Hungary (36.8 %), Bulgaria (36.9 %) and Slovakia (39.0 %).
Services related to long-term nursing care accounted for less than 10.0 % of current healthcare expenditure in more than half of the EU Member States for which data are available, but for almost a quarter of the total spend in the Netherlands (24.2 %) and Denmark (24.4 %). It should be noted that the relatively low share reported for many EU Member States could well be due to the main burden of long-term nursing care residing with family members with no payment being made for providing these services. In addition, limitations within the data compilation exercise also make it difficult to separate the medical and social components of expenditure for long-term nursing care, leading to an inevitable impact on cross-country comparisons.
The proportion of current healthcare expenditure incurred by ancillary services to healthcare (such as laboratory testing or the transportation of patients) varied significantly among EU Member States, ranging from 1.9 % in the Netherlands to 8.8 % in Portugal, with Cyprus (9.4 %) and Estonia (11.1 %) above this range. Similarly, expenditure related to prevention and public health programmes exhibited large discrepancies between EU Member States. In both cases these figures are likely to provide an under-estimate of the true values, as part of the expenditure on these services is attributed to medical treatment and as such may be recorded under the heading of curative care. Expenditure on healthcare administration and health insurance was generally lower in those EU Member States with centralised social security systems or those EU Member States where private insurance plays a relatively restricted role, ranging from 1.5 % of current healthcare expenditure or less in Sweden, Denmark and Bulgaria, through to 5.5 % in Cyprus and Germany and 7.0 % in France.
Healthcare expenditure by provider
An analysis of current healthcare expenditure by provider is shown in Table 3. Hospitals generally accounted for the highest share of current healthcare expenditure, ranging from 25.8 % of the total in Slovakia to more than 45.0 % in Denmark, Sweden and Estonia. The second most important category was that of ambulatory care providers, its share ranging from 14.2 % of current healthcare expenditure in Romania to more than 30.0 % in Germany, Belgium, Portugal, Cyprus and Finland. The share of various retail establishments and other providers of medical goods in current healthcare expenditure varied by a factor of three — with the lowest shares, below 15.0 %, being recorded in Sweden, the Netherlands, Denmark and Luxembourg. Most of the EU Member States reported that retail establishments and other providers of medical goods accounted for a share of current healthcare expenditure ranging between 16.0 % and 30.9 %, a share that rose above 36.0 % in Hungary, Bulgaria and Slovakia. However, it should be borne in mind that healthcare providers classified under the same group do not necessarily perform the same set of activities. Hospitals, for example, may, in addition to inpatient services, offer outpatient, ancillary or other types of service.
Non-expenditure data on healthcare
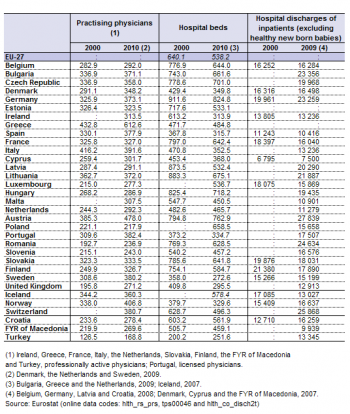
High demand for healthcare staff in some EU Member States may result in qualified resources moving from one country to another. One of the key indicators for measuring healthcare staff is the total number of physicians (head count), expressed per 100 000 inhabitants. In this context, Eurostat gives preference to the concept of practising physicians (although data are not available for six EU Member States — being replaced by the number of professionally active physicians in Ireland, Greece, France, the Netherlands and Slovakia, and by the number of licensed physicians in Portugal) — see Table 4.
In 2010, the highest number of practising physicians per 100 000 inhabitants was recorded in Austria (478.0), followed by Sweden (380.2, 2009 data), while Norway (406.8) and Switzerland (380.7) also recorded relatively high ratios; note that Greece and Portugal also reported a relatively high number of professionally active and licensed physicians. Between 2000 and 2010 the number of physicians per 100 000 inhabitants increased in the majority of EU Member States (incomplete data for Ireland, Italy and Malta), although modest reductions were recorded in Slovakia, Estonia and Poland. The reduction of practising physicians in these Member States may be explained by breaks in the data series — for example, from 2004 onwards the Polish data excludes private practices (thought to account for about 2 000 physicians).
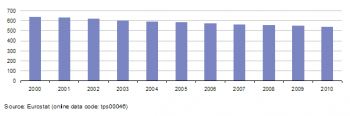
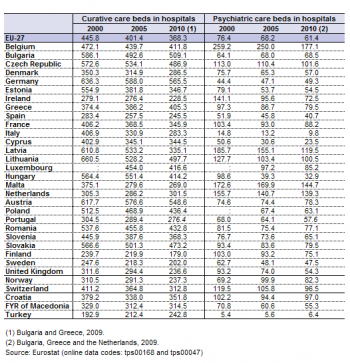
The number of hospital beds per 100 000 inhabitants averaged 538.2 in the EU-27 in 2010. The reduction in bed numbers between 2000 and 2010 across the whole of the EU-27 was equal to 101.9 beds per 100 000 inhabitants. Among the EU Member States, this ratio ranged from 272.6 beds per 100 000 inhabitants in Sweden to 824.8 in Germany; among the non-member countries for which data are available Turkey (251.6) was the only country outside this range. During the 10 years between 2000 and 2010, the number of hospital beds per 100 000 inhabitants fell in every Member State, except Greece (incomplete data for Luxembourg and Poland). The largest reductions in the availability of hospital beds were recorded in the three Baltic Member States, Ireland, the United Kingdom, Italy, Sweden and Finland. These reductions may reflect, among others, economic constraints, increased efficiency through the use of technical resources (for example, imaging equipment), a general shift from inpatient to outpatient operations, and shorter periods spent in hospital following an operation. It should also be noted that there were breaks in the time series for Sweden and the United Kingdom.
A closer look at the availability of hospital beds, identifying curative care beds and psychiatric beds — see Table 5, shows a reduction in numbers for both types of beds between 2000 and 2010, with the EU-27 average falling to 368.3 curative care beds and 61.4 psychiatric care beds. The reduction was reproduced in each of the EU Member States for which data are available, except for an increase in the number of curative care beds in Greece and the number of psychiatric beds in Bulgaria (2000 to 2009), Germany and Austria. It should be noted that there were breaks in the time series for Bulgaria and Germany.
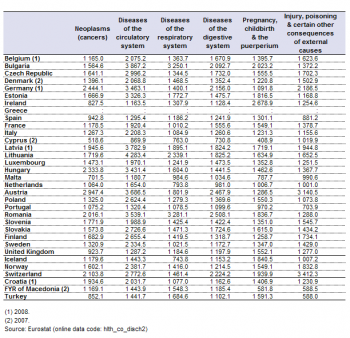
In terms of healthcare activity, diseases of the circulatory system often accounted for the highest number of hospital discharges in 2010 — see Table 6. One quarter of the EU Member States for which data are available reported in excess of 3 000 discharges per 100 000 inhabitants for diseases of the circulatory system. The average length of a hospital stay was generally highest among those patients suffering from cancer or problems relating to the circulatory system — see Table 7.
Data sources and availability
Eurostat, the Organisation for Economic Cooperation and Development (OECD) and the World Health Organisation (WHO) have established a common framework for a joint healthcare data collection. Following this framework, EU Member States submit their data to Eurostat on the basis of a gentlemen’s agreement. The data collected relates to:
- healthcare expenditure following the methodology of the system of health accounts (SHA);
- statistics on human and physical resources in healthcare — supplemented by additional Eurostat data on hospital activities (discharges and procedures).
Monetary and non-monetary statistics may be used to evaluate how a country’s healthcare system responds to the challenge of universal access to good healthcare, through measuring financial, human and technical resources within the healthcare sector and the allocation of these resources between healthcare activities (for example, preventive and curative care), groups of healthcare providers (for example, hospitals and ambulatory centres), or healthcare professionals (for example, medical and paramedical staff).
Healthcare expenditure
Healthcare data on expenditure are based on various surveys and administrative (register-based) data sources, as well as estimations made within the EU Member States, reflecting country-specific ways of organising healthcare and different reporting systems for the collection of statistics pertaining to healthcare.
Total current healthcare expenditure quantifies the economic resources of both the public and private sectors dedicated to healthcare, with the exception of those related to capital investment. It reflects current expenditure of resident units on the final consumption of goods and services directed at improving the health status of individuals and of the population.
The SHA provides a framework for interrelated classifications and tables relating to the international reporting of healthcare expenditure and financing. The set of core SHA tables addresses three basic questions: i) who finances healthcare goods and services; ii) which healthcare providers deliver them, and; iii) what kinds of healthcare goods and services are consumed. Consequently, the SHA is organised around a tri-dimensional system for the recording of health expenditure, by means of the international classification for health accounts (ICHA), defining:
- healthcare expenditure by financing agents (ICHA-HF) — which provides an analysis of public and private units that directly pay providers for their provision of healthcare goods and services;
- healthcare expenditure by provider (ICHA-HP) — which classifies units contributing to the provision of healthcare goods and services such as hospitals, various outpatients settings, diagnosis centres or retailers of medical goods;
- healthcare expenditure by function (ICHA-HC) — which details the split in healthcare expenditure following the purpose of healthcare activities — such as, health promotion, curing illnesses, rehabilitation or long-term care.
Data coverage is close to 100 % for the first-digit level of each of the three core classifications, but ranges between 75 % and 85 % at the second-digit level. However, it is possible that despite relatively high rates of coverage, there may be departures from the standard classifications. Expenditure reported under some of these ICHA categories may be under or overestimated and it is recommended to refer to specific country metadata before analysing the data.
Non-expenditure data on healthcare
Non-expenditure healthcare data are mainly based on administrative national sources; a few countries compile this information from surveys. As a consequence, the information collected is not always comparable. Information on the non-expenditure component of healthcare can be divided into two broad groups of data:
- resource-related healthcare data on human, physical and technical resources, including staff (such as physicians, dentists, nursing and caring professionals, pharmacists and physiotherapists) and hospital beds;
- output-related data that focuses on hospital patients and their treatment(s), in particular for inpatients.
Hospitals are defined according to the classification of healthcare providers within the SHA; all public and private hospitals should be covered.
Data on healthcare staff, in the form of human resources available for providing healthcare services, are provided irrespective of the sector of employment (in other words, regardless of whether the personnel are independent, employed by a hospital, or any other healthcare provider). Three main concepts are used for health professionals: practising, professionally active and licensed. Practising physicians provide services directly to patients; professionally active physicians include those who practise as well as those working in administration and research with their medical education being a pre-requisite for the job they carry out; physicians licensed to practise are those entitled to work as physicians plus, for example, those who are retired.
Hospital bed numbers provide information on healthcare capacities, in other words on the maximum number of patients who can be treated by hospitals. Hospital beds (occupied or unoccupied) are those which are regularly maintained and staffed and immediately available for the care of admitted patients. This indicator should ideally cover beds in all hospitals, including general hospitals, mental health and substance abuse hospitals, and other specialty hospitals. The statistics should include public as well as private sector establishments — although some EU Member States provide data only for the public sector — for example, Denmark (psychiatric beds), Ireland (total and curative beds), Cyprus (curative and psychiatric beds) and the United Kingdom. Curative care (or acute care) beds are those that are available for curative care; these form a subgroup of total hospital beds.
Output-related indicators focus on hospital patients and cover the interaction between patients and healthcare systems, generally through the form of the treatment they receive. Data are available for a range of indicators including hospital discharges of inpatients and day cases by age, gender, and selected (groups of) diseases; the average length of stay of inpatients; or the medical procedures performed in hospitals. The number of hospital discharges is the most commonly used measure of the utilisation of hospital services. Discharges, rather than admissions, are used because hospital abstracts for inpatient care are based on information gathered at the time of discharge.
Context
Health outcomes across the EU are strikingly different according to where people live, their ethnicity, sex and socioeconomic status. The EU promotes the coordination of national healthcare policies through an open method of coordination which places particular emphasis on the access to, and the quality and sustainability of healthcare. Some of the main objectives include: shorter waiting times; universal insurance coverage; affordable care; more patient-centred care and a higher use of outpatients; greater use of evidence-based medicine, effective prevention programmes, generic medicines, and simplified administrative procedures; and strengthening health promotion and disease prevention.
Access to healthcare, the introduction of technological progress and greater patient choice is increasingly being considered against a background of financial sustainability. Many of the challenges facing governments across the EU were outlined in the European Commission’s White paper titled ‘Together for health: a strategic approach for the EU 2008–2013’ (COM(2007) 630 final). In February 2013, the European Commission adopted a Communication titled ‘Towards social investment for growth and cohesion’ (COM(2013) 83 final). The main axis of the Communication include: ensuring that social protection systems respond to people’s needs at critical moments throughout their lives; simplified and better targeted social policies, to provide adequate and sustainable social protection systems; and upgrading active inclusion strategies in the Member States. Concerning health, the Communication notes the differences in the accessibility to and quality of healthcare between Member States as well as underlining the need for reforms of healthcare systems with the twin aim to ensure access to high quality healthcare and to use public resources more efficiently. In the context of social investment throughout an individual’s lifetime, the Communication notes that investing in health, starting from an early age, allows people to remain active longer and in better health, raises the productivity of the workforce and lowers the financial pressures on healthcare systems.
See also
- Health introduced
- Healthcare expenditure
- Health statistics at regional level
- The EU in the world - health
Further Eurostat information
Publications
- European social statistics, 2013 edition
- Health in Europe — Data 1998–2003, 2006 edition
- Health statistics — Key data on health 2002 — Data 1970–2001
Main tables
- Health status (t_hlth_state)
- Health care, see:
- Health care (t_hlth_care)
Database
- Health status (hlth_state)
- Health determinants (hlth_det)
Dedicated section
- Health, see:
Methodology / Metadata
- Health care expenditure (ESMS metadata file - hlth_sha_esms)
- Health care: resources and patients (non-expenditure data) (ESMS metadata file - hlth_care_esms)
Source data for tables and figures (MS Excel)
External links
- European Commission Directorate General for health and consumers — Public health
- OECD — Health policies and data
- World Health Organisation (WHO) — Health systems
Notes
- ↑ Denmark and the Czech Republic: 2010. Latvia: 2009. Bulgaria, Cyprus and Luxembourg: 2008.