Data extracted in July 2024.
Planned article update: September 2025.
Highlights
3.6% of all deaths in the EU in 2021 resulted from mental and behavioural disorders.
In 2021, dementia was the most common cause of death from mental and behavioural disorders in the EU.
In 2021, there were 3.1 million in-patients with mental and behavioural disorders who were discharged from hospitals in 24 of the EU countries for which data are available.
(per 100 000 inhabitants)
Source: Eurostat (hlth_cd_asdr2)
This article presents an overview of European Union (EU) statistics related to mental and behavioural disorders and intentional self-harm (which is an external cause of morbidity and mortality). Mental and behavioural disorders include, for example, dementia (a chronic or persistent mental health condition characterised by memory loss, personality changes and impaired reasoning), schizophrenia and psychoactive substance use disorders (such as alcohol or drug dependence). This article covers deaths from mental and behavioural disorders, healthcare for mental and behavioural disorders, as well as the availability of specialist healthcare resources (hospital beds and healthcare personnel) for the treatment of mental and behavioural disorders.
This article is 1 of a set of statistical articles concerning healthcare activities in the EU which forms part of an online publication on Health in the European Union – facts and figures.
Deaths from mental and behavioural disorders and intentional self-harm
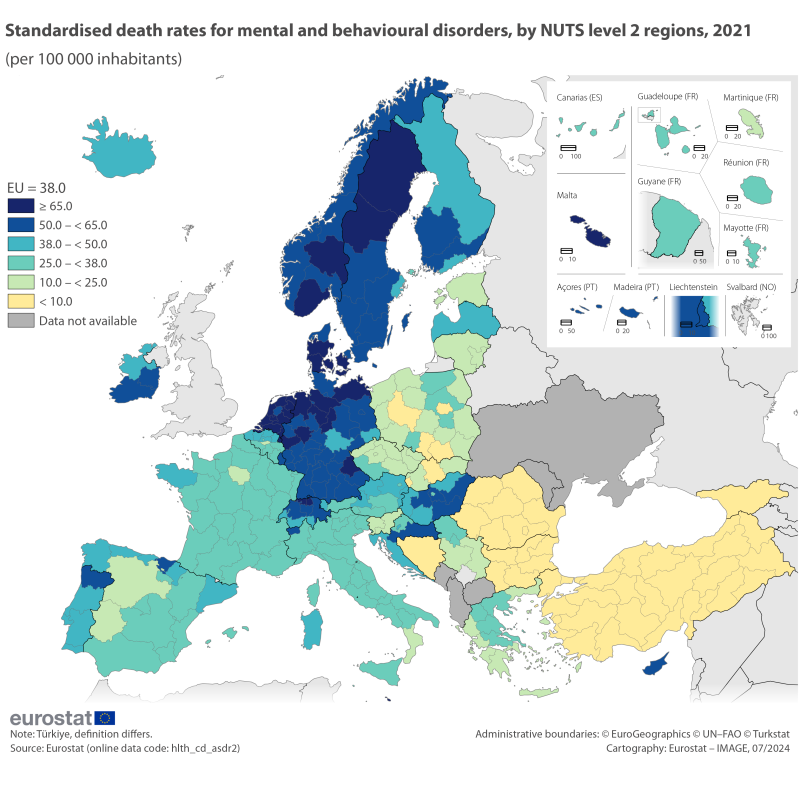
In 2021, there were 190 900 deaths in the EU resulting from mental and behavioural disorders, equivalent to 3.6% of all deaths. Relative to the population size, there were 38 deaths from mental and behavioural disorders per 100 000 inhabitants.
Mental and behavioural disorders were a particularly common cause of death at advanced ages. The EU standardised death rate from mental and behavioural disorders in 2021 for those aged 65 years or over was 42 times as high as the standardised death rate for people aged less than 65 years. This can be compared with the same ratio for all causes of death, where the death rate for those aged 65 years or over was 21 times as high.
Among mental and behavioural disorders, dementia was the most common cause of death in the EU among those aged 65 years or over
(per 100 000 inhabitants)
Source: Eurostat (hlth_cd_asdr2)
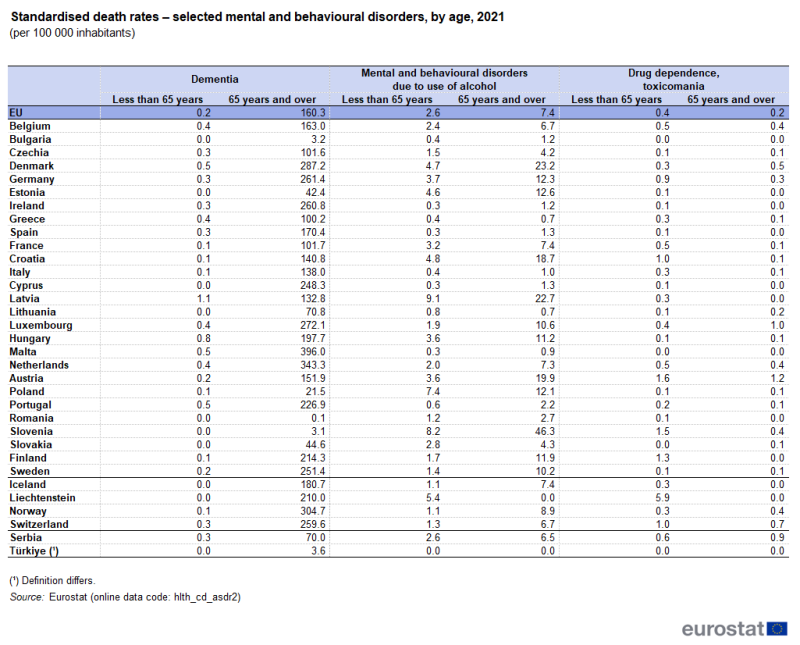
A more detailed analysis of causes of death for a selection of mental and behavioural disorders is presented in Table 1. The leading cause of death from mental and behavioural disorders was dementia, which accounted for 84% of all deaths from mental and behavioural disorders in the EU in 2021. The standardised death rate for dementia was 160 deaths per 100 000 people aged 65 years or over in 2021; this was 697 times higher than the standardised death rate for dementia among those aged less than 65 years (0.2 per 100 000).
The highest standardised death rate for dementia in those aged 65 years or over was recorded in Malta (396.0 deaths per 100 000 elderly inhabitants in 2021), followed by the Netherlands (343.3 deaths). The lowest standardised death rates were reported in Romania, Slovenia and Bulgaria – all under 4.0 deaths from dementia per 100 000 elderly inhabitants – while the next lowest rate was in Poland (21.5 deaths).
The 2nd leading cause of death from mental and behavioural disorders across the EU in 2021 was due to the use of alcohol. This was also the leading cause of death from mental and behavioural disorders in those aged less than 65 years, with 2.6 deaths per 100 000 in the EU in 2021. The use of alcohol accounted for 61% of all deaths from mental and behavioural disorders among people aged less than 65 years. Latvia reported the highest standardised death rate from mental and behavioural disorders due to the use of alcohol in this age group (9.1 deaths per 100 000 inhabitants aged less than 65 years), while Slovenia had the highest rate for people aged 65 years or over (46.3 deaths per 100 000 elderly inhabitants). The standardised death rate from mental and behavioural disorders due to the use of alcohol is higher among people aged 65 years or over in all the EU countries except for Lithuania.
In 2021, the only mental and behavioural disorder in the EU for which the standardised death rate was higher among those aged less than 65 years was drug dependence, also known as toxicomania. An analysis by country shows that in both age groups the standardised death rate for toxicomania ranged between 0.0 and 1.6 deaths per 100 000 inhabitants for both age groups. The standardised death rate was higher for those aged less than 65 years in a majority of EU countries (17 out of 27), while 6 countries had similar rates for both age groups. Luxembourg, Denmark, Lithuania and Slovakia were the exceptions, as they were the only EU countries where the standardised death rate was higher among people aged 65 years and over.
Males were 3.7 times as likely as females to die from intentional self-harm
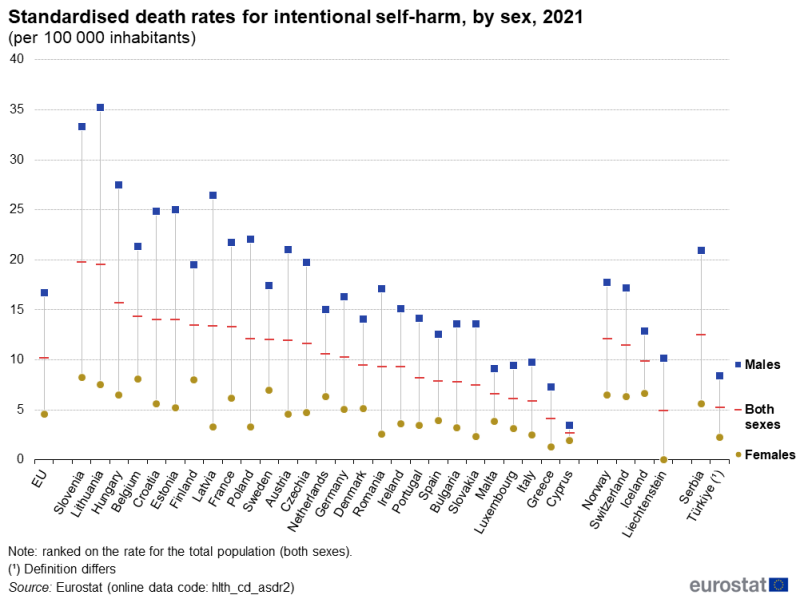
In 2021, the standardised death rate for intentional self-harm (ICD-10 codes X60 to X84 and Y87.0) was 10.2 per 100 000 inhabitants for the EU, with the rate for males 3.7 times as high as that for females (see Figure 1). It should be noted that the comparability of data on intentional self-harm is thought to be limited due to an under-reporting of suicides in some EU countries (possibly due to cultural stigma among other reasons).
(per 100 000 inhabitants)
Source: Eurostat (hlth_cd_asdr2)
Across the EU countries, the highest standardised death rate for intentional self-harm in 2021 was recorded for Slovenia (19.8 per 100 000 inhabitants), followed closely by Lithuania (19.5 per 100 000 inhabitants). Rates between 5.9 and 15.7 per 100 000 inhabitants were recorded for most of the other EU countries, although Greece (4.2 per 100 000 inhabitants) and Cyprus (2.7 per 100 000 inhabitants) were below this range.
In all EU countries in 2021, the standardised death rate for intentional self-harm was higher for males than for females, ranging from 1.8 times as high in Cyprus to 8.0 times as high in Latvia. The largest difference was recorded in Lithuania, where the rate for females was 7.5 per 100 000 female inhabitants and the rate for males was 35.2 per 100 000 male inhabitants.
Mental healthcare
In 2021, there were 3.1 million in-patients with mental and behavioural disorders who were discharged from hospitals in the EU countries for which data are available (2020 data for Malta; no recent data for Denmark, Greece or Luxembourg). In Germany, there were 1.2 million in-patient discharges among people treated for mental and behavioural disorders in 2021. There were only 2 other EU countries which recorded in excess of 200 000 in-patient discharges – France and Poland – while these diseases accounted for less than 10 000 in-patient discharges in Ireland, the Netherlands, Malta (2020 data) and Cyprus.
Relative to population size, Germany recorded the highest number of in-patient discharges for mental and behavioural disorders in 2021, with 1 463 discharges per 100 000 inhabitants. Latvia, Finland, Austria and France also recorded more than 1 000 in-patient discharges for mental and behavioural disorders per 100 000 inhabitants. The ratio in Germany was 36 times as high as the equivalent ratio for the Netherlands, where the lowest rate was recorded (40.1 in-patient discharges per 100 000 inhabitants) and 22 times as high as the equivalent ratio for Cyprus, where the next lowest rate was recorded (67.9 in-patient discharges per 100 000 inhabitants). In the other EU countries for which data are available, this rate was between 153 and 908 in-patient discharges per 100 000 inhabitants.
Figure 2 shows the breakdown of discharges by diagnosis, for mental and behavioural disorders. In 2021, dementia accounted for the smallest proportion of hospital discharges in 19 of the 23 EU countries for which data are available, ranging from 1.4 discharges per 100 000 inhabitants in the Netherlands up to 126.6 discharges per 100 000 inhabitants in Finland.

(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)
In 2021, mental and behavioural disorders due to alcohol and/or psychoactive substance use accounted for 24% of hospital discharges relating to mental and behavioural disorders in the EU (2020 data for Malta; no data for Denmark, Estonia, Greece or Luxembourg). Relative to the population size, the highest number of discharges from mental and behavioural disorders due to alcohol and/or psychoactive substance use was reported in Latvia with 485.7 hospital discharges per 100 000 inhabitants. The lowest number of discharges were reported in the Netherlands (9.9 discharges per 100 000 inhabitants) and Cyprus (3.6 discharges per 100 000 inhabitants). In the other EU countries for which data are available, this figure ranged from 18 to 381 discharges per 100 000 inhabitants, with Portugal at the lower end and Germany at the upper end of this range.
In 2021, schizophrenia, schizotypal and delusional disorders accounted for 16% of hospital discharges from mental and behavioural discharges among the EU countries for which data are available (2020 data for Malta; no data for Denmark, Estonia, Greece or Luxembourg). The rate of discharges from schizophrenia, schizotypal and delusional disorders ranged from 281.0 discharges per 100 000 inhabitants in Latvia to 2.0 discharges per 100 000 inhabitants in the Netherland.
In 2021, mood (affective) disorders accounted for 25% of hospital discharges from mental and behavioural discharges among the EU countries for which data are available (2020 data for Malta; no data for Denmark, Estonia, Greece or Luxembourg). The highest rate was recorded in Germany, with 429.0 discharges from mood (affective) disorders per 100 000 inhabitants; the lowest rate was recorded in the Netherlands, with 1.7 discharges from mood (affective) disorders per 100 000 inhabitants.
Particularly long average length of stay for in-patients with mental and behavioural disorders
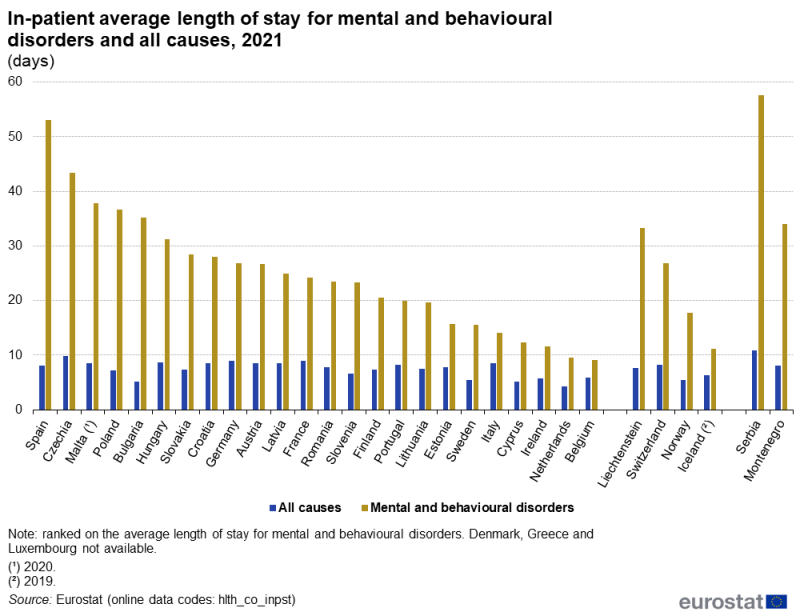
Figure 3 presents an analysis of the average length of hospital stays for in-patients treated for mental and behavioural disorders and for all causes in 2021. The average length of stay for in-patients treated for mental and behavioural disorders ranged from 9.1 days in Belgium and 9.5 days in the Netherlands up to 43.4 days in Czechia and 53.1 days in Spain.
In 2021, a large majority of the EU countries reported that the average length of stay for mental and behavioural disorders was the longest of all the conditions included in the International Shortlist for Hospital Morbidity Tabulation (ISHMT). In Cyprus, longer average stays were recorded for certain conditions originating in the perinatal period, while in Italy a longer average was recorded for COVID-19. The average length of stay for in-patients treated for mental and behavioural disorders was 6.8 times as high as the average for all causes in Bulgaria and was 1.5 times as high as the average for all causes in Belgium.
(days)
Source: Eurostat (hlth_co_inpst)
Healthcare beds and personnel
In 2022, there were 321 500 psychiatric care beds in EU hospitals, equivalent to 14% of all hospital beds.
Figure 4 presents data for the number of psychiatric care beds in hospitals relative to the size of population. In 2022, Belgium reported the highest ratio with 140.7 psychiatric care beds per 100 000 inhabitants, followed by Germany, with 131.3 per 100 000 inhabitants. Italy (8.1 per 100 000 inhabitants) and Cyprus (18.6 per 100 000 inhabitants) were the only EU countries to report fewer than 20.0 psychiatric care beds per 100 000 inhabitants. In the other EU countries, the number of psychiatric care beds ranged between 30.3 and 108.5 per 100 000 inhabitants.
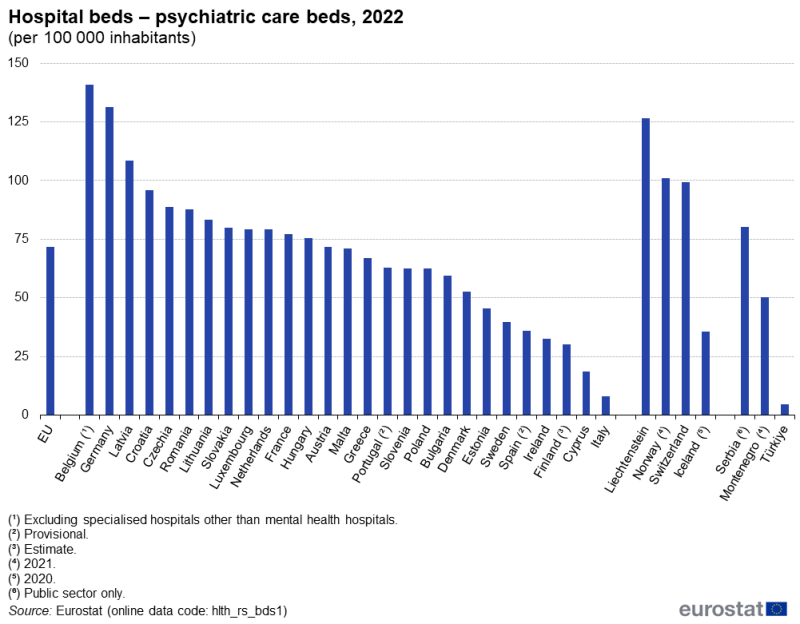
(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_bds1)
Increasing numbers of psychiatrists in most EU countries
Relative to the population size, the number of psychiatrists rose between 2012 and 2022 in the vast majority of EU countries. There was an increase recorded in 21 of the 24 EU countries for which data are available (only partial data for Luxembourg and Hungary; no recent data for Slovakia). The biggest increases were in Greece and Malta, where the number of psychiatrists increased, respectively, by 8.5 and 7.7 per 100 000 inhabitants. By contrast, Latvia, Finland (2012–20) and Sweden (2012–21) all recorded relatively small falls in their number of psychiatrists relative to population size.
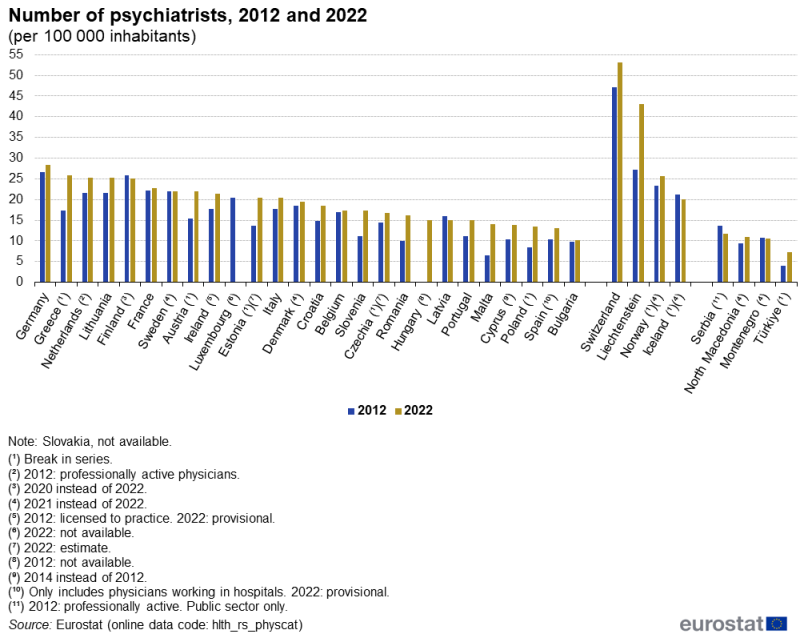
(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_physcat)
Source data for tables and graphs
Key concepts
Data sources
An in-patient is a patient who is formally admitted (or ‘hospitalised’) to an institution for treatment and/or care and stays for a minimum of 1 night or more than 24 hours in the hospital or other institution providing in-patient care. An in-patient or day care patient is discharged from hospital when formally released after a procedure or course of treatment (episode of care). A discharge may occur because of the finalisation of treatment, signing out against medical advice, transfer to another healthcare institution, or because of death.
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised (rather than crude) death rate can be compiled which is independent of the age and sex structure of a population. This is done as most causes of death vary significantly by age and according to sex and the standardisation facilitates comparisons of rates over time and between countries[1].
Mental and behavioural disorders are often highly stigmatised and diagnostic criteria for different mental and behavioural disorders often have many overlapping symptoms making diagnoses difficult and variable. Consequently, mental and behavioural disorders are known to be under-diagnosed, or under-reported as cause of death. Furthermore, coding practices may vary significantly between countries [2].
Statistics on causes of death provide information on mortality patterns, supplying information on developments over time in the underlying causes of death. This source is documented in more detail in this article on causes of death statistics - methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Statistics on causes of death are based on death certificates established by medical experts assessing the underlying cause of death. Note there is a difference in the coding of cases where the mental and behavioural disorder was the established underlying cause of death, as distinguished from cases where a death occurred for someone who was suffering from a mental and behavioural disorder at the time of death.
Causes of death are currently classified according to the 86 causes in the European shortlist, which is based on the International Statistical Classification of Diseases and Related Health Problems (ICD) 10th revision. Chapter V (F00-F99) of the ICD covers mental and behavioural disorders and Chapter XX (V01-Y89) covers external causes of mortality (including intentional self-harm). For the purpose of this article the following ICD-10 codes were covered for the described causes of death:
- F01, F03 for Dementia. Please note that Alzheimer disease (ICD-10 code: G30) is not included in this selection;
- F10 for Alcohol abuse (including alcoholic psychosis);
- F11-F16, F18-F19 for Drug dependence, toxicomania;
- X60-X84, X87.0 for Suicide and intentional self-harm.
Statistics on healthcare resources (such as beds and personnel) and healthcare activities (such as information on hospital discharges) are documented in this article onHealthcare non-expenditure statistics - methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For hospital discharges and the length of stay in hospitals, the International Shortlist for Hospital Morbidity Tabulation (ISHMT) is used to classify data from 2000 onwards; Chapter V covers mental and behavioural disorders:
- dementia (0501);
- mental and behavioural disorders due to alcohol (0502);
- mental and behavioural disorders due to use of other psychoactive substances (0503);
- mood [affective] disorders (0504);
- schizophrenia, schizotypal and delusional disorders (0505);
- other mental and behavioural disorders (0506).
For country specific notes, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
The Healthcare non-expenditure statistics manual provides an overview of the classifications, both for mandatory variables and variables provided on a voluntary basis.
Tables in this article use the following notation
| Value in italics | estimate or provisional data |
| Value is – | not relevant or not applicable |
| Value is : | not available |
<context>
Context
Mental and behavioural disorders make up 1 of the largest categories of diseases in the EU. In 2021, the number of in-patient bed days for mental and behavioural disorders in the EU was 83.3 million (2020 data for Malta; no data for Denmark, Greece or Luxembourg), which was the largest number among all categories of diseases and conditions, ahead of diseases of the circulatory system. Nevertheless, it is believed that many mild to moderate mental disorders are under-diagnosed and consequently untreated and not reported within the available official statistics.
As well as being important for individuals, good mental health is important for society. Mental health issues impact economic performance through productivity losses and increased work-disability costs and may also create a burden for educational and justice systems.
Contributing to the European Year of Youth (2022), and as part of the EU4Health 2022 work plan, 2 new projects aim to improve the mental health of children, young people and their families through the implementation of best practice. The practices concerned are:
- a sport-based support programme to improve life skills and social, psychological and emotional resources among socially vulnerable children and adolescents;
- a 2-step intervention to support mental health and well-being of young people and their families in vulnerable situations.
Mental health and neurological disorders are included as 1 of the 5 main strands covered by the European Commission’s Healthier together – EU non-communicable diseases (NCD) initiative. The initiative was launched in December 2021 and aims to support EU countries in identifying and implementing effective policies and actions to reduce the burden of major NCDs and improve citizens’ health and well-being.
The European Commission has also mobilised €9 million from the EU4Health programme to help people fleeing Ukraine in urgent need of mental health and trauma support.
In 2023, the European Commission added a pillar to the European Health Union for a comprehensive approach to mental health. It aims to put mental health on a par with physical health and to ensure a new, cross-sectoral approach to mental health issues[3]. With 20 flagship initiatives and €1.23 billion in EU funding from different financial instruments, the European Commission will support EU countries making people and their mental health a priority. Under this initiative, the EU will take a holistic approach to mental health, based on 3 guiding principles
- adequate and effective prevention
- access to high quality and affordable mental healthcare and treatment
- reintegration into society after recovery.
</context>
Footnotes
- Standard Population report: https://ec.europa.eu/eurostat/en/web/products-manuals-and-guidelines/-/ks-ra-13-028 ↑
- OECD/European Union (2018), Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris/European Union, Brussels, https://doi.org/10.1787/health_glance_eur-2018-en. ↑
- Official Commission Communication: https://health.ec.europa.eu/document/download/cef45b6d-a871-44d5-9d62-3cecc47eda89_en?filename=com_2023_298_1_act_en.pdf ↑
Explore further
Other articles
Online publications
Causes of death
Healthcare activities
Methodology
General health statistics articles
Database
- Health (hlth), see
- Health care (hlth_care)
- Health care resources (hlth_res)
- Health care staff (hlth_staff)
- Health care facilities (hlth_facil)
- Health care activities (hlth_act)
- Hospital discharges and length of stay for inpatient and curative care (hlth_co_dischls)
- Hospital discharges - national data (hlth_hosd)
- Length of stay in hospital (hlth_hostay)
- Health care resources (hlth_res)
- Causes of death (hlth_cdeath)
- General mortality (hlth_cd_gmor)
- Causes of death - deaths by country of residence and occurrence (hlth_cd_aro)
- Causes of death - standardised death rate by NUTS 2 region of residence (hlth_cd_asdr2)
- General mortality (hlth_cd_gmor)
- Health care (hlth_care)
Thematic section
Publications
Selected datasets
Methodology
Manuals and guidelines
Metadata
- Causes of death (SIMS metadata file – hlth_cdeath_sims)
- Health care resources (ESMS metadata file – hlth_res_esms)
