Archive:Healthcare statistics
- Data from September 2008, most recent data: Further Eurostat information, Main tables and Database.
Most Europeans agree that there is a basic need for universal access to healthcare, as the cost of many modern-day health treatments can often be prohibitive to the average individual. The systems for providing healthcare vary considerably among European Union (EU) Member States, although widespread use is made of public provision (regional or national health services) and comprehensive healthcare insurance. Healthcare schemes generally cover the entire resident population; nevertheless, an increasing proportion of individuals choose to belong to private insurance schemes (usually in addition to the national provision for care). This article presents some basic statistics on healthcare across the EU, including the number of physicians and how these have changed, the number of hospital beds and the most common illnesses that fill them, and the amount of time patients spend in hospitals.
Main statistical findings
Healthcare expenditure
Current expenditure on healthcare in 2006 ranged from PPS 403 per inhabitant in Romania to more than PPS 2 700 per inhabitant in Germany, France, Belgium, the Netherlands, Austria (2004), Denmark and Sweden; note that no data is available for six of the Member States. In nearly all of the Member States expenditure was greatest for care provided by hospitals, while a significant proportion of healthcare expenditure was for providers of ambulatory healthcare, as well as for retail sale and other providers of medical goods.
An analysis of the functions of healthcare expenditure show that curative care generally accounted for around half of all healthcare expenditure. Medical goods for outpatients was generally the second largest function, with around one quarter of total expenditure, although it exceeded one third in Slovakia, Bulgaria, Hungary and Lithuania. Rehabilitative care was generally 4 % or less of the total, with the 11 % share in Cyprus an exception among those Member States with data available. Long-term nursing care accounted for less than 10 % of expenditure in the majority of the Member States, but reached 22 % in Denmark.
Sources of financing varied considerably, reflecting the variety of health systems in place across the Member States. In several countries, three fifths or more of healthcare expenditure is financed from social security funds: the highest shares were in the Czech Republic (81 %) and the Netherlands (77 %). Other government financing was the main source in Denmark and Sweden at more than four fifths of the total, while more than half of the financing in Portugal, Spain, Finland and Latvia also came from this source. The other major source of funds was direct payments, referred to as ‘out-of-pocket’ expenditure, which ranged from less than 10 % of the total in the Netherlands and France, to over two fifths in Bulgaria and Latvia (2004), and nearly half the total in Cyprus. Private insurance enterprises generally contributed a small share of healthcare finance, only surpassing 10 % of the total in Slovenia (13.8 %) and France (13.1 %).
Non-expenditure data on healthcare
As Table 4 shows, the highest number of physicians per 100 000 inhabitants was recorded in Belgium (405 practising physicians in 2008) followed by Austria (374 practising physicians in 2008); note, however, that methodological differences occur between the various types of physicians reported in some countries. Between 1997 and 2007 the number of physicians per 100 000 inhabitants increased in the majority of Member States, although reductions were recorded in Italy, Hungary, Poland and Lithuania; the slight fall in Estonia may be due to methodological reasons.
The number of hospital beds per 100 000 inhabitants in 2007 ranged from 288 in Sweden to 829 in Germany. During the ten years between 1997 and 2007, the number of hospital beds per 100 000 inhabitants fell in every Member State for which data is available, except in Malta. The largest reductions in the availability of hospital beds were recorded in Luxembourg, Bulgaria, Sweden, the Baltic Member States and Italy. A more detailed breakdown shows that reductions in bed numbers were spread across different categories, with an average of 390 curative care beds available per 100 000 inhabitants in the EU-27 in 2007, while there were 55 psychiatric beds in hospitals per 100 000 inhabitants; when compared with 1998, these latest figures represent overall reductions in bed numbers of 22.3 % and 26.8 % respectively.
The general reduction in hospital bed numbers may result from a more efficient use of resources, with an increasing number of operations handled by out-patient treatment, and shorter periods spent in hospital following an operation. Nevertheless, the output of each national health service, as measured by the number of in-patient discharges, will usually (at least to some degree), reflect the number of physicians and hospital beds available. As Table 4 shows, the highest number of hospital discharges in 2007 was recorded in Austria (more than 27 000 per 100 000 inhabitants), which was almost 25 % more than the next highest figure (22 100 discharges in Lithuania). At the other end of the range, the number of hospital discharges of in-patients was relatively low in both Malta (2004) and Cyprus (2007), both below 8 000 per 100 000 inhabitants.
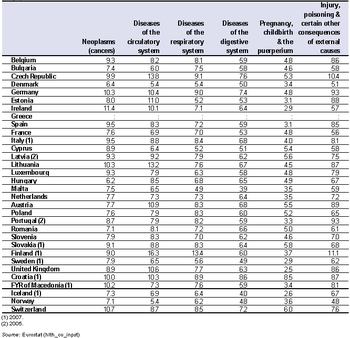
Circulatory system diseases accounted for the highest number hospital discharges in 2007 in the vast majority of countries for which data are available, often with upwards of 3 000 discharges per 100 000 inhabitants (Table 6). However, in Romania higher numbers of discharges were recorded for respiratory system diseases, while in Ireland and Spain there were more discharges from pregnancies and related diagnosis, and in Cyprus the highest number of discharges resulted from injury or poisoning. Cyprus had a particularly low level of hospital discharges, which may in part be due to patients travelling abroad for specialist treatment; indeed, this trend may also be significant for other Member States.
The average length of hospital stay was generally longest for those patients suffering from cancer or from circulatory system problems (Table 6). The average time spent in hospital is a function of hospital efficiency, as well as the type of treatments available.
Data sources and availability
Healthcare expenditure
According to the System of Health Accounts (SHA), healthcare expenditure data can be analysed by type of provider, by function (goods and services) and by financing agent. Healthcare data on expenditure are based on various information sources including surveys and administrative data sources. The country-specific way of organising and financing healthcare, existing departures from SHA definitions and information gaps justify the fact that data are not always completely comparable between countries. To collect data on healthcare expenditure, the system of health accounts (SHA) and its related set of international classification for health accounts (ICHA) is used. The SHA is organised around a tri-axial system for recording health expenditure, defining healthcare financing agents, functions and service providers.
Mechanisms of healthcare financing are becoming increasingly complex in many countries with a wide range of institutions involved. At least a basic subdivision of public and private financing is reported in many cases. A detailed breakdown of expenditure on health by financing agents is an essential component of a comprehensive SHA.
Healthcare in a country comprises the sum of activities performed either by institutions or individuals pursuing, through the application of medical, paramedical and nursing knowledge and technology, the purposes/core functions of:
- promoting health and preventing disease;
- curing illness and reducing premature mortality;
- caring for persons affected by chronic illness who require nursing care;
- caring for persons with health-related impairment, disability, and handicaps who require nursing care;
- assisting patients to die with dignity;
- providing and administering public health;
- providing and administering health programs, health insurance and other funding arrangements.
Health-related functions such as the education and training of the health workforce, research and development in health, and environmental health should be distinguished from the core functions; as far as possible they should be excluded when measuring activities belonging to core healthcare functions.
Non-expenditure data on healthcare
Information on healthcare can be divided into two broad groups of data:
- resource-related healthcare data on human and technical resources;
- output-related data that focuses on hospital patients and the treatment(s) they receive.
Healthcare data are largely based on administrative data sources, and, to a large degree, they reflect country-specific ways of organising healthcare; as such, the information collected may not always be completely comparable.
Hospitals are defined according to the classification of healthcare providers of the System of health accounts (SHA); all public and private hospitals should be covered. Data on healthcare staff, in the form of human resources available for providing healthcare services, is provided irrespective of the sector of employment (i.e. whether the personnel are independent, employed by a hospital, or any other healthcare provider). These statistics cover healthcare professionals such as physicians, dentists, nurses, pharmacists and physiotherapists.
In the context of comparing healthcare services across Member States, Eurostat gives preference to the concept of ’practising professionals’, as this best describes the availability of healthcare resources. By way of example, physicians may be counted as licensed, economically active or practising. Data for two or more concepts are available in the majority of Member States. The preference, however, is for practising physicians, or those seeing patients either in a hospital, practice or elsewhere. Practising physicians’ tasks include:
- conducting medical examinations and making diagnoses;
- prescribing medication and giving treatment for diagnosed illnesses, disorders or injuries;
- giving specialised medical or surgical treatment for particular types of illnesses, disorders or injuries;
- giving advice on and applying preventive medicine methods and treatments.
Hospital bed numbers provide information on healthcare capacities, i.e. on the maximum number of patients who can be treated by hospitals. Hospital beds are those which are regularly maintained and staffed and immediately available for the care of admitted patients. These include: beds in all hospitals, including general hospitals, mental health and substance abuse hospitals, and other specialty hospitals: occupied and unoccupied beds. The statistics exclude surgical tables, recovery trolleys, emergency stretchers, beds for same-day care, cots for healthy infants, beds in wards which were closed for any reason, provisional and temporary beds, or beds in nursing and residential care facilities. They cover beds accommodating patients who are formally admitted (or hospitalised) to an institution for treatment and/or care and who stay for a minimum of one night. Curative care (or acute care) beds are those that are available for curative care; these form a subgroup of total hospital beds.
Output-related indicators focus on hospital patients and covers the interaction between patients and healthcare systems, namely in the form of the treatment received. Data in this domain are available for a range of indicators including hospital discharges of in-patients and day cases by age, sex, and selected (groups of) diseases; the average length of stay of in-patients; or the medical procedures performed in hospitals; the number of hospital discharges is the most commonly used measure of the utilisation of hospital services. Discharges, rather than admissions, are used because hospital abstracts for in-patient care are based on information gathered at the time of discharge. A hospital discharge is defined as the formal release of a patient from a hospital after a procedure or course of treatment. A discharge occurs whenever a patient leaves because of finalisation of treatment, signs out against medical advice, transfers to another healthcare institution or on death. Healthy newborn babies should be included, while patient transfers to another department within the same institution are excluded.
Context
A new health strategy ‘Together for health: a strategic approach for the EU 2008-2013’ was adopted on 23 October 2007, putting in place a framework to improve health in the EU through a value-driven approach, recognising the links between health and economic prosperity, integrating health in all policies, and strengthening the EU’s voice in global health.
The provision of healthcare varies considerably within the EU, although widespread use is made of public provision and comprehensive healthcare insurance. Healthcare schemes generally cover all residents; nevertheless, an increasing proportion of individuals choose to adhere to private insurance schemes (usually on top of the national provision for care).
Public regulation of the healthcare sector is a complex task, as the healthcare market is characterised by numerous market imperfections. EU Member States generally aim to balance the efficient use of resources with ensuring that healthcare provisions are available to all. There is no simple answer to the question of how much a country should spend on healthcare, as each Member State faces a different disease burden, while populations have different expectations of what services their national healthcare systems should offer. Indeed, the amount of money needed to fund a healthcare system is a function of several variables, the most obvious being the burden of disease requiring treatment. However, there is no simple linear relationship between the burden of disease and the need for resources, as some conditions can be treated simply and at low cost while others may require a complex and expensive care.
The main consumers of healthcare are older people – a section of the European population that is growing rapidly, partly as a result of ageing baby-boomers, but also because of continued increases in life expectancy. The likely increase in numbers of elderly persons will probably drive demand for more healthcare provision in the future. Medical advances are also likely to result in more and better treatments being available. Demand for healthcare is also likely to rise in the coming years in relation to long-term care provision (nursing and convalescence homes).
In addition, more patients are travelling across borders to receive treatment, to avoid waiting lists or to seek specialist treatment that may only be available abroad. The EU works towards ensuring that people who move across borders have access to healthcare anywhere within the Union. Indeed, healthcare systems and health policies across the EU are becoming more interconnected. This is not only a result of the movement of patients and professionals between countries, but may also be attributed to a set of common public expectations of health services across Europe, as well as more rapid dissemination of new medical technologies and techniques. On 2 July 2008, as part of a 'Renewed social agenda', the European Commission adopted a draft directive on the application of patients’ rights to cross-border healthcare.
Further Eurostat information
Publications
Main tables
- Health, see:
- Public health
- Main tables
- Public health (t_hlth)
- Health care: resources and patients (non-expenditure data) (t_hlth_care)
- Public health (t_hlth)
- Main tables
Database
- Health, see:
- Public health
- Database
- Public health (hlth)
- Health care expenditure (hlth_sha)
- Health care: resources and patients (non-expenditure data) (hlth_care)
- Health care: indicators from surveys (SILC, HIS round 2004) (hlth_care1)
- Public health (hlth)
- Database