3. How hard is it measure?
- 3.1 Factors affecting blood pressure measurement
- 3.2 Blood pressure measurements in routine clinical practice
- 3.3 Blood pressure measurements in epidemiological / observational studies
- 3.4 Mercury sphygmomanometers
3.1 Factors affecting blood pressure measurement
It is important to be aware of the factors that affect blood pressure measurement (Rose 1965):
(1) The technical skills of the observer;
(2) The inherent variability of blood pressure;
(3) The accuracy of the device, including its limitations and applications;
(4) The difficulty in measuring blood pressure in some special groups, e.g. the elderly, patients with arrhythmias, patients with a large arm, children, pregnant women.
The most important element in using auscultatory methods is the observer. All observers need adequate training in listening and recognising the correct sounds. Most common sources of error in many reports are mostly due to the observer, including poor hearing, difficulty/failure in interpreting the Korotkov sounds and lack of concentration. Most serious errors involve the interpretation of the Korotkov sounds and recognising diastolic pressure. Observers may be influenced by the subjects. For example, observers tend to be reluctant in diagnosing young healthy subjects as hypertensive or obese older persons as normotensive when the blood pressure is around 140/90 mmHg (systolic/diastolic blood pressure) resulting in a tendency to under read in the first case and over estimate in the latter. Observer-related issues include: prejudice and bias such as threshold avoidance; terminal digit preference; fast deflation, etc. (Beevers et al. 2001).
To accurately measure blood pressure, the following important criteria have to be applied, irrespective of what type of device is being used.
- Posture of the patient supine, sitting or standing.
- Cuff at heart level and arm supported; if not supported, isometric exercise is performed and will result in recording a higher blood pressure.
- The use of correct cuff and bladder size for the appropriate arm/leg size. Over cuffing (use of a bladder that is too large) will lead to under estimation of blood pressure, and under cuffing (use of a bladder that is too small) will over estimate the blood pressure.
- Measurement of the blood pressure on both arms at first visit to help identify consistent difference in blood pressure between the arms.
- Accuracy of the device; the device should be well maintained, in pristine condition, calibrated as per the manufacturer’s instructions and validated according to accepted standards using appropriate protocols.
3.2 Blood pressure measurements in routine clinical practice
Repeated office blood pressure measurements are mandatory in clinical practice to characterise precisely the blood-pressure-related cardiovascular risk of individual subjects. Precise recommendations are available to ensure standardised accurate measurements (O’Brien et al. 2003, Parati et al. 2008a), which until now have been obtained in most cases through the auscultatory technique making use of mercury or aneroid sphygmomanometers. Given the fact that aneroid manometers easily lose calibration, mercury manometers have been, until now, the recommended tools for auscultatory blood pressure readings, on which the conventional management of hypertensive patients has been based over the last 60-70 years. In more recent years an increasing use of home blood pressure monitoring and 24-hour ambulatory blood pressure monitoring has been observed (both based on oscillometric blood pressure measurements), aimed at complementing the information provided by office blood pressure measurements. This is based on the evidence of a stronger prognostic value of 24-hour ambulatory and home blood pressure monitoring as compared to isolated office readings (Parati et al. 2008b, Parati et al. 2009b, Verdecchia et al. 2009). A slow progressive increase in the use of oscillometric blood pressure measuring devices at the time of the office visit has been recently observed, although auscultatory readings are still preferred by physicians in most countries.
There are a number of physiological and pathological states that may influence the ability of an oscillometric device to obtain an equivalent reading to a mercury sphygmomanometer. Oscillometric measurements are dependant on movement, and changes in the amplitude of this movement, in the artery, and therefore maybe altered. Oscillometric measurements cannot be relied on in patients with arrhythmias, or some valvular heart disease such as aortic incompetence. Other patients with altered vascular compliance, such as diabetics, or the elderly, could have less accurate blood pressure readings using oscillometric measurement. Changes in vascular compliance may also be confounded by oedema, intravascular volume, hyperdynamic circulation and by changes in cardiac output such as pre-eclampsia, in which oscillometric readings frequently underestimate the blood pressure (Shennan and De Greeff 2007). Although the accuracy and reproducibility of Korotokov sounds in these disease states are not known, listening to the Korotkov sounds remains the technique in which current knowledge of indirect blood pressure is determined, and therefore, the auscultatory method of blood pressure is recommended in such populations.
3.3 Blood pressure measurements in epidemiological/observational studies
Very comprehensive research on population blood pressure exists throughout the world. These studies are essential for defining hypertension prevalence, awareness and treatment in any geographical region/country. A change in population blood pressure of 2 mmHg in systolic blood pressure translates to a change in stroke mortality of ten percent and coronary heart disease mortality of seven percent (Lewington et al. 2002). Therefore, data on progression from normotension to prehypertension and hypertension are very important in epidemiological research. The data have documented that prehypertension carries an increased risk for cardiovascular morbidity and mortality, and a high risk for progression to sustained hypertension (Hansen et al. 2007a, Julius et al. 2006). In this respect, changes from normotension to prehypertension are as important as the observation of hypertension itself. Reliable data are heavily dependent on blood pressure measurements carried out meticulously by properly trained personnel and with precise equipment. For this, adherence to a standardised technique over time is crucial. Findings of changes in population blood pressure are only meaningful if they are ascertained to be true differences and not related to a change in methods applied.
Nearly all results on population blood pressure have been obtained by the use of a standard mercury sphygmomanometer by well-trained health personnel (Cutler et al. 2008). Despite this, the readings are not without observer bias and end-digit preference. In an attempt to minimise observer bias and end-digit preference, a number of highly recognized epidemiological research institutions have used the Random Zero Mercury Sphygmomanometers, where the reader has to subtract a random chosen magnitude of mmHg (from 0 to 20 mmHg) at the very end of the measurement. Despite minimising observer bias, the equipment has been shown to slightly underestimate the "true” blood pressure level as obtained by the use of a standard mercury manometer (Yang et al. 2008). Another approach that has been employed is the "London School of Hygiene Sphygmomanometers” (Andersen and Jensen 2007) where the reader is blinded to the mercury column but has to tap a button when they hear the first and the fourth Korotkov sounds (phase 1 and phase 5). In recent years, 24-hour ambulatory blood pressure measurements have been introduced in population studies and comprehensive databases have been constructed, e.g. the Idaco Database on population studies with contributions from many parts of the world (Hansen et al. 2007b). All these studies have convincingly shown that 24-hour ambulatory blood pressure measurements determined with oscillometric devices (at approximately 80 readings over 24 hours), are superior for prediction of cardiovascular morbidity and mortality as compared to a few measurements of blood pressure performed in clinical conditions with a standard mercury sphygmomanometer. In almost all these studies, although not exclusively, the comparator has been the standard mercury sphygmomanometer (Hansen et al. 2007b).
Research into normal values for home blood pressure and the prognostic implication is less comprehensive. This research has been almost exclusively carried out with automatic oscillometric devices, with measurements being compared to the mercury sphygmomanometer. Data are accumulating showing that the predictive prognostic value of a certain number of home blood pressure readings is superior to a single or a few blood pressure readings performed in a clinic using a mercury sphygmomanometer (Sega et al. 2005). The home readings are a reflection of more precise estimation of the actual blood pressure levels over many readings as compared to few readings in the clinical setting. So far, comparisons of measurements obtained with mercury sphygmomanometer versus oscillometric automatic devices, obtained in the same clinical setting for determination of population blood pressure and prognostic implications, are missing. However, in the Pamela Study, three clinic readings with a mercury sphygmomanometer were compared to two home blood pressure oscillometric readings (Sega et al. 2005). As expected, the clinical readings were somewhat higher, but the prognostic implication was not that much different.
In long-term outcome clinical trials, usually running for three to five years, mercury sphygmomanometers have been used as the gold standard for office blood pressure measurement. In some recent trials (the HOT Study, the ASCOT Study and the OnTarget Study) automatic oscillometric devices were used (Dahlöf et al. 2005, Hansson et al. 1998, Yusuf et al. 2008). In some of these studies it was shown that small differences in measured blood pressure already can have an impact on cardiovascular diseases.
There is rapidly growing information on normal values and the prognostic implications of 24 hour ambulatory blood pressure measurements with oscillometric devices, while knowledge on self/home blood pressure measurements with oscillometric devices is less substantial. So far, a direct comparison between clinic blood pressure and prognostic implication based on measurements carried out with mercury sphygmomanometer and those with automatic oscillometric devices is lacking.
In conclusion, the vast majority of information on population blood pressure (secular trends, progression to hypertension and prognostic implications, and also the benefits from treatment-induced blood pressure reduction in terms of cardiovascular events prevention) has so far been obtained with the use of mercury sphygmomanometers. Reliable data on changes in population blood pressure level, incidence and prevalence of hypertension, awareness and treatment, derived from follow-up studies are dependent on the use of consistent and trustworthy methods. It can be expected that epidemiological/observational studies in the future will comprise repetitive blood pressure measurements at home carried out with well-calibrated, well-validated automatic oscillometric equipment. For the moment, mercury sphygmomanometers are essential for such validation of newly developed blood pressure measurement devices. Otherwise, the conclusions based on the results of long–term epidemiological studies on changes in population blood pressure may be seriously jeopardised.
3.4 Mercury sphygmomanometers
The mercury-containing sphygmomanometer should not be viewed as an absolute standard. It is however, with all its faults as an indirect blood pressure determination, the method used to establish our current knowledge. Since Riva-Rocci’s times mercury sphygmomanometers associated with the occlusion-auscultatory technique have been used in clinical and epidemiological studies on hypertension. They represent the cornerstone for cardiovascular disease prognosis and prevention, as well as in the daily clinical management of patients with high blood pressure. As a result of this time- honoured use, blood pressure values are still quantified in mmHg both in current practice and in research, and doctors keep watching the mercury column as the most faithful indicator of the blood pressure levels in their patients. A commonly perceived advantage of mercury manometers lies in the fact that, when they are well maintained (see below), they offer "absolute” measurements of blood pressure, and represent a "gold standard” reference technique used to validate all other methods which provide information on blood pressure levels in mmHg without using a mercury column. The blood pressure measurement based on the mercury sphygmomanometer is an indirect blood pressure determination, and is difficult to perfectly mimic with other techniques unrelated to auscultation of Korotkov sounds.
3.4.1 Characteristics
The high-density of liquid mercury metal provides an acceptable short length of the rising column for visualization of the pressure in the cuff. Therefore, the mercury column in a sphygmomanometer is used as a simple, gravity-based unit. When properly maintained and serviced and when used by knowledgeable trained health professionals, it can give accurate indirect measurements of both systolic and diastolic pressure. Currently it is considered to be the most accurate technique (O'Brien et al. 2003).
A complete mercury sphygmomanometer requires a cuff, bladder, tubing and a rubber bulb, and should be maintained in good condition and serviced regularly according to the manufacturers’ instructions. Mercury sphygmomanometers are easily checked and maintained, but great care should be taken when handling mercury. The revised European Standard (EN 1060 series) recommends that mercury sphygmomanometers display a warning to this effect (CEN 1995a).
3.4.2 Limitations
Despite its widespread availability for almost a century, there can be major problems with the use of mercury sphygmomanometers in clinical practice. Reports from hospitals and family practices have suggested that many mercury sphygmomanometers are defective because of poor maintenance (Beevers and Morgan 1993, Burke et al. 1982, Feher et al. 1992, Gillespie and Curzio 1998, Hutchinson et al. 1994, Markandu et al. 2000, Wingfield et al. 1996).
Moreover, several studies have shown that there is a lack of knowledge of the technical aspects of the actual blood pressure measurement in both doctors and nurses and other health care professionals who use the mercury sphygmomanometers. The reports also suggest that the technique of blood pressure measurement is not applied very well. Additionally, there is a lack of knowledge of the appropriate blood pressure equipment and how to maintain the devices so that they are calibrated and in pristine condition. One should be aware of the fact that issues of maintenance are a factor for every blood pressure measurement device.
There are several other limitations of using the auscultatory method which affect both mercury and aneroid manometers:
- Terminal digit preference: Tendency of the observer to round off the number to their choosing e.g. 144/96 mmHg as 140/100 mmHg or 150/90 mmHg (systolic/diastolic blood pressure). This is the zero preference. The observer finds it easier to read the prominent larger 10 mmHg markings instead of the smaller, 2 mmHg markings.
- Errors may occur when the manometer is not kept vertical (see fig. 1), and the device is rested on the side of the bed or, having it tilted against the pillow. This is an issue when the device is being used at the patient’s bedside, not when used for public- health monitoring. Positioning of the Hg manometer
- positioning of the Hg manometer (see above) dynamic response of the Hg column (see below) clearness of the display
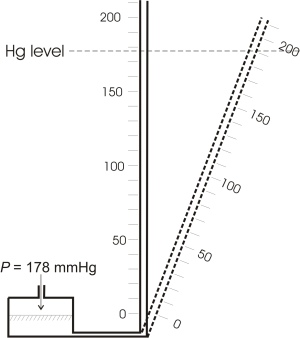
Figure 1: Measurement error due to incorrect positioning of the Hg manometer. In this diagram the incorrect positioning of the tube results in a measurement error of ca. 12 mmHg.
- Inflation/deflation system: Another important limitation to consider is the performance of the inflation/deflation system and of the occluding bladder encased in a cuff, and proper application of auscultation with a stethoscope. Those issues apply to all blood pressure measuring devices using the auscultatory method.
The inflation/deflation system consists of an inflating and deflating mechanism connected by rubber tubing to an occluding bladder. The standard mercury sphygmomanometers used in clinical practice are operated manually, with inflation being effected by means of a bulb compressed by hand and deflation by means of a release valve, which is also controlled by hand. The pump and control valve are connected to the inflatable bladder and thence to the sphygmomanometer by rubber tubing. Leaks from cracked or perished rubber make accurate measurement of blood pressure difficult because the fall of the mercury cannot be controlled. The length of tubing between the cuff and the manometer should be at least 70 cm and that between the inflation source and the cuff should be at least 30 cm. Connections should be airtight and easily disconnected.
In addition, technical (maintenance) problems may exist such as:
(i) Oxidisation of the mercury is another very common occurrence, which can increase with time and make the columns difficult to read.
(ii) The markings on the column also fade with time, again making it impossible to read accurately.
(iii) Dynamic response
3.4.3 Technical accuracy of Hg sphygmomanometers
The mercury manometers incorporate the (non SI unit) mmHg as a read-out system. The use of this manometer does not automatically guarantee that the cuff pressure measurement is always correct. In 1952, the Physikalisch-Technische Bundesanstalt in Germany issued requirements for these sphygmomanometers on a voluntary basis. The International Organisation of Legal Metrology published its first International Recommendation (IR 16) in 1973 and at approximately the same time national standards and similar documents were published in several countries such as the USA and Switzerland. Since then, these documents have been updated several times. To support the "Council Directive 93/42/EEC concerning medical devices” the European standards organisation CEN developed a standard (EN 1060, part 1-4) between 1995 and 2004 (CEN 1995a, 1995b, 1997, 2004), which became a harmonized standard in that framework. Recently the international standard organisations ISO and IEC jointly developed standards to test sphygmomanometers; they were published between 2007 and 2009 (IEC 2009, ISO 2007). These standards are expected to replace the CEN standards in the near future.
Regarding the accuracy of Hg manometer there are three main aspects to be considered:
Since the technical accuracy of the Hg manometer is affected by the inclination relative to gravity, means need to be provided to ensure the correct positioning of the reservoir and the tube, e.g. a water-level. Figure 1 illustrates the effect of incorrect positioning on the accuracy. According to ISO 81060-1 (ISO, 2007) a portable Hg manometer "shall be provided with an adjusting or locking mechanism to secure it in the position for use as indicated in the accompanying documents”.
To prevent the spillage of Hg the ISO 81060-1 standard requires the following: The Hg manometer shall incorporate a stopping device at the top of the tube that
- permits both the inward and outward flow of air, and
- prevents the passage of liquid mercury.
The reservoir shall also be fitted with a stopping device to prevent the Hg from flowing out of the reservoir neck and into the attached tubing and permits the inward and outward flow of air.
When the passage of air is limited owing to contamination or deterioration of the stopping devices, the falling pressure is displayed with some delay by the mercury column in the tube. This delay prevents the user from reading the correct pressure value; when measuring during cuff pressure deflation, there will be a systematic error resulting in too high blood pressure values.
Consequently the metrological test of a Hg manometer has to include The following list summarises the technical features determining the accuracy of mercury sphygmomanometers (O’Brien et al. 2003).
Features affecting accuracy of the mercury sphygmomanometer:
- The top of the mercury meniscus should rest at exactly zero without pressure applied; if it is below, add mercury.
- The scale should be clearly calibrated in 2 mm divisions from 0 to 300 mmHg and should indicate accurately the differences between the levels of mercury in the tube and in the reservoir.
- The diameter of the reservoir must be at least ten times that of the vertical tube, or the vertical scale must correct for the drop in the mercury level in the reservoir as the column rises.
- Substantial errors may occur if the manometer is not kept vertical during measurement. Calibrations on floor models are especially adjusted to compensate for the tilt in the face of the gauge. Stand-mounted manometers are recommended for hospital use. This allows the observer to adjust the level of the sphygmomanometer and to perform measurement without having to balance the sphygmomanometer precariously on the side of the bed.
- The air vent at the top of the manometer must be kept patent, as clogging will cause the mercury column to respond sluggishly and to overestimate pressure.
- The control valve is one of the most common causes of error in sphygmomanometers and when it becomes defective it should be replaced. Spare control valves should be available in hospitals and a spare control valve should be supplied with sphygmomanometers.
Les droits d’auteur de la Structure à Trois Niveaux utilisée pour communiquer cet avis du CSRSEN appartiennent à Cogeneris SPRL.