Healthcare personnel statistics - physicians
Data extracted in July 2023.
Planned article update: July 2024.
Highlights
There were an estimated 1.82 million practising physicians across the EU in 2021.
In 2021, more than half of all physicians in Italy and Bulgaria were aged 55 years and over.
In 2021, more than two-thirds of the total number of physicians in Latvia, Estonia, Lithuania and Romania were women.
The number of graduating medical doctors per 100 000 inhabitants rose between 2011 and 2021 in nearly all of the EU Member States; Austria was the only exception among those countries for which data are available.
Number of general medical practitioners, 2021
This article presents an overview of European Union (EU) statistics on physicians. It provides information on specialist healthcare personnel, as well as data on the number and ratio of graduates in this field (note that all physicians need to possess a degree in medicine).
Physicians are licensed to provide services to patients as consumers of health care. They give advice, conduct medical examinations, diagnose diseases and conditions, apply preventive medical methods, prescribe medication, treat illnesses and provide specialised medical or surgical treatment.
This article is one of a set of statistical articles concerning healthcare resources in the EU which forms part of an online publication on health statistics.
Full article
Healthcare personnel
For physicians, Eurostat collects data for three concepts:
- 'practising' - physicians providing services directly to patients;
- 'professionally active' - 'practising' physicians plus physicians for whom their medical education is a prerequisite for the execution of their job;
- 'licensed' - physicians who are registered and entitled to practise as physicians.
In this article preference is given to the concept of 'practising' physicians which is also used for the European core health indicator (ECHI) on physicians. For some EU Member States, data are not available for this concept and therefore data are presented for one of the alternative concepts instead: notes indicate these exceptions in each table and figure.
There were an estimated 1.82 million physicians working in the EU
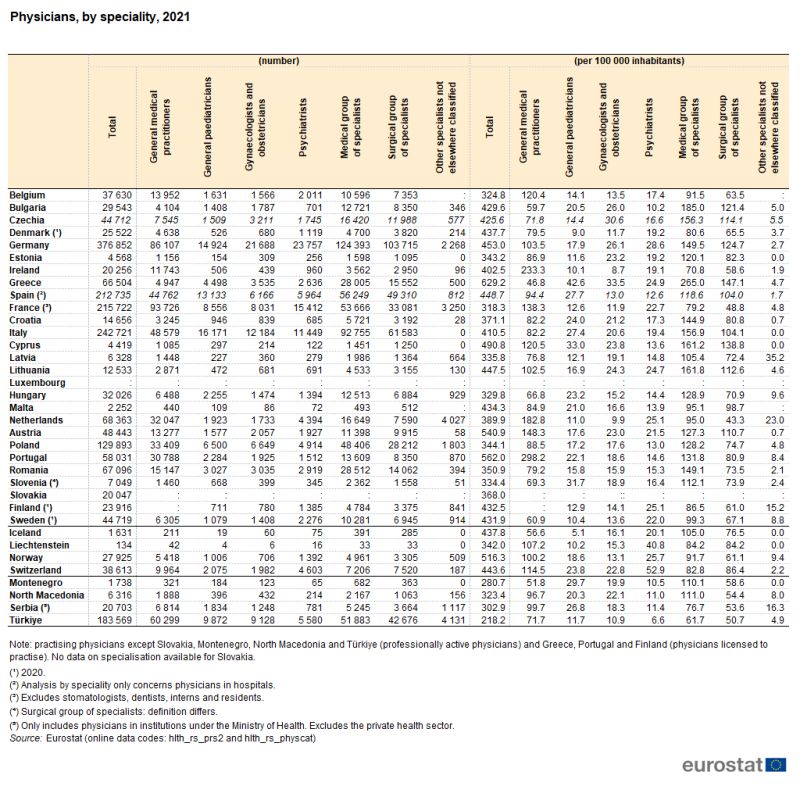
In 2021, there were an estimated 1.82 million practising physicians in the EU (see Table 1 footnotes for more details). The highest overall numbers of practising physicians were recorded in the largest EU Member States: Germany (377 000, equivalent to 20.7 % of the EU total), followed at some distance by Italy (243 000), France (216 000) and Spain (213 000). Together, these four Member States accounted for 57.7 % of the total number of practising physicians in the EU. The next highest number of practising physicians was in Poland, 130 000, equivalent to 7.2 % of the EU total.
Greece had the highest number of physicians per 100 000 inhabitants
Among the EU Member States, Greece (physicians licensed to practise) recorded the highest number of physicians relative to population size, at 629.2 per 100 000 inhabitants in 2021. This was considerably higher than in any of the other EU Member States; Portugal (562.0 physicians licensed to practise per 100 000 inhabitants) and Austria (540.9 practising physicians per 100 000 inhabitants) had the next highest ratios. By contrast, the lowest ratio was 318.3 practising physicians per 100 000 inhabitants in France.
In the vast majority of EU Member States, there were more medical specialists than general medical practitioners
Generalist medical practitioners do not limit their practice to certain disease categories or methods of treatment and may assume responsibility for the provision of continuing and comprehensive medical care to individuals, families and communities. By contrast, medical specialists include doctors who specialise in the diagnosis and non-surgical treatment of physical disorders and diseases, for example specialists in internal medicine, cardiology, oncology and radiology. Surgical specialists include doctors who specialise in the use of surgical techniques to treat disorders and diseases, for example, specialists in general surgery, neurological surgery, anaesthesiology or accident and emergency medicine.
A closer examination of the data in Table 1 reveals that in 2021, there were approximately 469 000 generalist medical practitioners (GPs) across the EU (excluding data for Luxembourg, Slovakia and Finland). The highest number of GPs was recorded in France (94 000), followed by Germany (86 000), while Portugal (physicians licensed to practise) and Ireland reported the highest number of GPs per 100 000 inhabitants (298.2 and 233.3 per 100 000 inhabitants, respectively). In 2021, the proportion of physicians who were GPs was highest in Ireland (58 %), Portugal (53 %) and the Netherlands (47 %).
There were 18 EU Member States (among 24 for which recent data are available) where there were more medical specialists than GPs in 2021. The Member States with the highest number of medical specialists were Germany (124 000) and Italy (93 000). Greece reported the highest number of medical specialists per 100 000 inhabitants (265.0 per 100 000 inhabitants, licensed to practice), followed by Bulgaria (185.0 per 100 000 inhabitants).
In 2021, there were more surgical specialists than GPs in half the 24 EU Member States for which data are available. Once again, the highest numbers of surgical specialists were reported in Germany (104 000) and Italy (62 000). Greece reported the highest number per 100 000 inhabitants (147.1 per 100 000 inhabitants), followed by Cyprus (138.8 per 100 000; 2020 data). Malta was the only Member State to report more surgical specialists (512) than either medical specialists (493) or GPs (440).
The number of physicians per 100 000 inhabitants rose in nearly all EU Member States between 2016 and 2021
The number of physicians per 100 000 inhabitants increased in nearly all of the EU Member States between 2016 and 2021 (see Figure 1); note that there are no recent data available for Luxembourg. The one exception was Estonia. Note that increases may result from a higher absolute number of physicians and/or from a smaller number of inhabitants. This increasing trend may reflect demographic shifts with ageing populations in Europe; as the proportion of older generations in the EU increased in recent years, demand for health and social care services also increased.
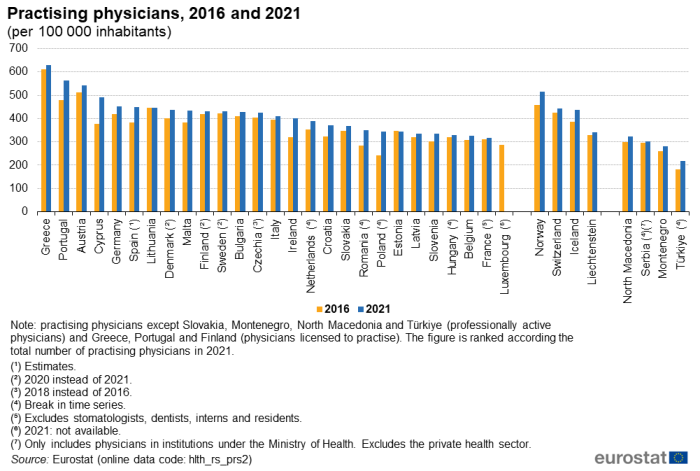
(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_prs2)
Leaving aside EU Member States which recorded a break in time series, the largest relative increase was recorded in Cyprus, where the number of physicians rose from 376.8 per 100 000 inhabitants in 2016 to 344.1 per 100 000 inhabitants in 2021 (an overall increase of 30.2 %). By contrast, the lowest increase was 0.2 % in Lithuania, while in Estonia there was a fall of 0.7 %.
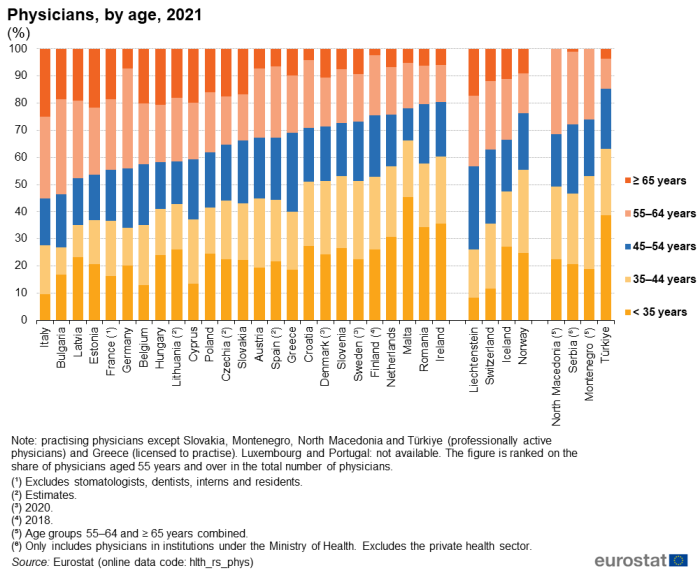
Italy had the largest share of physicians aged 55 years and over
There has been a rapid ageing of the (healthcare) workforce across much of the EU as the baby-boomer generation is reaching retirement age. In 10 EU Member States, the share of physicians aged 55 years and over was over 40.0 % in 2021. Among these, the share was over 50.0 % in Italy and Bulgaria (55.2 % and 53.6 %, respectively). In most of the remaining Member States for which data are available, the relative importance of this age group in the total number of physicians was between 24.3 % and 38.2 %; lesser shares were recorded in Malta (21.9 %), Romania (20.4 %) and Ireland (19.7 %). Reflecting these small shares for physicians aged 55 years and over, the highest proportions of younger physicians (under 35 years) were in Malta (45.5 %), Ireland (35.5 %) and Romania (34.4 %).
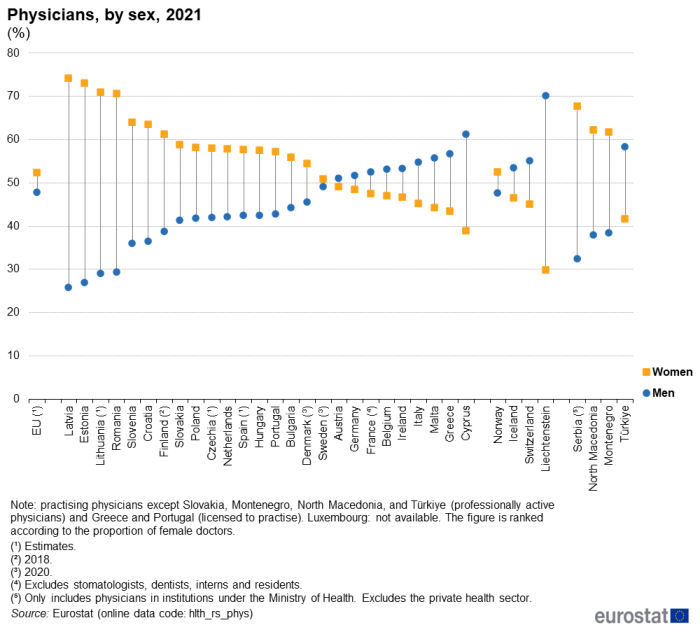
More than two-thirds of the total number of physicians in Latvia, Estonia, Lithuania and Romania were women
The analysis presented in Figure 3 shows that there were considerable differences between EU Member States with respect to each sex's share of the total number of physicians. Over the last decade, the overall proportion of female physicians increased gradually. By 2018, there was a slight majority of physicians in the EU who were female, and this proportion rose in the last three years to reach 52.2 %.
In 2021, a majority (17) of the 26 EU Member States for which data are available reported that they had a higher number of female than male physicians. In Finland (2018 data), Croatia and Slovenia, more than 60 % of all physicians were women, while in Romania and the Baltic Member States this proportion exceeded 70 %. The largest shares of female doctors were recorded in Estonia (73 %) and Latvia (74 %). By contrast, the greatest share of male physicians (61 %) was recorded in Cyprus. Relatively high proportions of male physicians were also recorded in Greece, Malta and Italy (all within the range of 55 % to 57 %). The smallest gaps between the shares of the two sexes – both 2 percentage points (pp) – were observed in Austria and Sweden (2020 data).
Health graduates
Some EU Member States face concerns over a forecasted lack of supply of physicians available to their healthcare workforces in the future. Among other actions, this has led some to promote measures designed to encourage more students to pursue medical degrees.
Figure 4 provides information on the number of medical doctors graduating per 100 000 inhabitants. In 2021, there were an estimated 15.3 medical doctors graduating in the EU for every 100 000 inhabitants. The highest ratios were recorded in Latvia (27.3 per 100 000 inhabitants), Romania (26.2 per 100 000 inhabitants), Ireland (26.0 per 100 000 inhabitants) and Malta (25.1 per 100 000 inhabitants). Most of the remaining EU Member States for which data are available recorded ratios of 11.0 to 22.7 medical doctor graduates per 100 000 inhabitants, although no medical students graduated in Luxembourg.
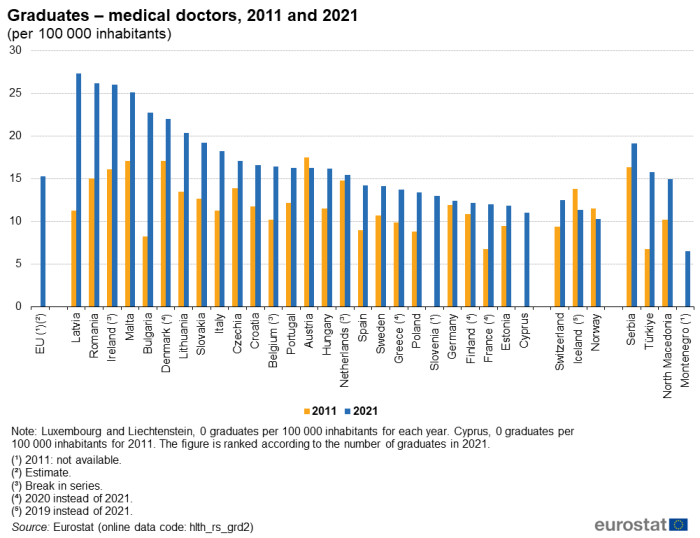
(per 100 000 inhabitants)
Source: Eurostat (hlth_rs_grd2)
A comparison between 2011 and 2021 shows that the number of medical doctors graduating per 100 000 inhabitants rose in nearly all of the EU Member States, the only exception being Austria which registered a relatively small decrease. The increase in most Member States may reflect a fall in the population and/or an increase in the number of graduates. In relative terms, the biggest increases were recorded in Latvia, Bulgaria, Romania and Cyprus.
Source data for tables and graphs
Data sources
Key concepts
Physicians are split into two broad occupational groups:
- generalist medical practitioners, which can, in turn, be divided into:
- general practitioners (GPs); and
- other generalist medical practitioners;
- specialist medical practitioners, which can, in turn, be subdivided into:
- medical specialists (doctors specialising in the diagnosis and non-surgical treatment of physical disorders and diseases);
- surgical specialists (doctors who specialise in the use of surgical techniques to treat disorders and diseases).
Practising physicians provide services directly to patients. They include people who have completed studies in medicine at university level and who are licensed to practise, be they salaried or self-employed, irrespective of the place of service provision. Unemployed physicians, retired physicians and students who have yet to graduate are excluded, as are physicians working in administration, research and other posts that exclude direct contact with patients.
Data on medical graduates for any given year cover the number of students who have graduated in medicine from medical faculties or similar institutions. The data exclude those who have graduated in pharmacy, dentistry/stomatology, or public health and epidemiology, as well as individuals who have completed post-graduate studies or training in medicine.
Healthcare resources
Statistics on healthcare resources (such as personnel and medical equipment) are documented in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For country specific notes on these data collections, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
Common definitions have been agreed between Eurostat, the OECD and the World Health Organisation (WHO) with respect to the employment of various healthcare professionals. Three main concepts are used to present this data; Eurostat gives preference to the concept of 'practising' physicians:
- 'practising', in other words, healthcare professionals providing services directly to patients;
- 'professionally active', in other words, 'practising' professionals plus healthcare professionals for whom their medical education is a prerequisite for the execution of their job;
- 'licensed', in other words, healthcare professionals who are registered and entitled to practise as healthcare professionals.
The Healthcare non-expenditure statistics manual provides an overview of the classifications, both for mandatory variables and variables provided on voluntary basis.
Symbols
In tables, a colon ':' is used to show where data are not available. Data in italics are estimates or provisional.
Context
Some health professionals seek jobs in other EU Member States: aside from the potential benefits for the individuals concerned, their movement can help rectify labour market imbalances between Member States. However, some Member States may experience important outflows of health professionals, which may exacerbate imbalances. Directive 2005/36/EC on the recognition of professional qualifications provides an EU-wide legal framework enabling Member States to recognise qualifications of health professionals from other Member States. A range of health professionals – including doctors – enjoy automatic recognition, in other words, if they are a certified practitioner in their home country then they are automatically entitled to practise anywhere else in the EU. The directive defines basic medical training as comprising a total of at least six years of university study or 5 500 hours of theoretical and practical training.
In the coming decades, population ageing is expected to be a major challenge for the EU's health sector. The demand for health care will probably increase substantially as a result of an ageing population and at the same time the proportion of the people in work will probably decline. As a result, staff shortages in certain medical specialisations or geographic areas may increase. In 2021, nearly two-fifths of all doctors in the EU were aged 55 years and over.
An action plan for the EU health workforce (SWD(2012) 093 final) seeks to help EU Member States tackle these challenges, by: improving workforce planning and forecasting; anticipating future skills' needs; improving the recruitment and retention of health professionals; and mitigating the negative effects of migration on health systems. Between 2013 and 2016, there was a joint action on health workforce planning and forecasting with 30 associated partners and 34 collaborative partners (from 28 European countries) working together on advancing the issue of planning and forecasting. Between 2017 and 2021, this work continued through SEPEN – Support for the health workforce planning and forecasting expert network, which released a series of technical reports and regular updates on the EU's health workforce.
The European Commission continues to initiate actions which seek to help EU Member States tackle this challenge under the EU4Health programme.
Direct access to
Online publications
Healthcare human and physical resources
Methodology
General health statistics articles
- Health (t_hlth)
- Health care (t_hlth_care)
- Health (hlth)
- Health care (hlth_care)
- Health care resources (hlth_res)
- Health care staff (hlth_staff)
- Health graduates (hlth_rs_grd2)
- Health personnel (hlth_rs_prs2)
- Physicians by category (hlth_rs_physcat)
- Physicians by sex and age (hlth_rs_phys)
- Health care staff (hlth_staff)
- Health care resources (hlth_res)
- Health care (hlth_care)
- Healthcare non-expenditure statistics (ESMS metadata file – hlth_res)
European Union, OECD and WHO
- European Commission – Public health, see:
- OECD – Health policies and data
- World Health Organisation (WHO), see:
Other external links