Effects of Biocides on antibiotic resistance
8. How can risks of resistance to both antibiotics and biocides be assessed?
- 8.1 What factors increase the risk of resistance to both biocides and antibiotics?
- 8.2 What (new) methods are required to effectively assess the risk of resistance?
Laboratory and field studies have shown that treating bacteria with low concentrations of biocide, leads to the preferred survival of resistant bacteria.
Antibiotic use is still the major cause of antibiotic resistance in clinical practice. Since antibiotic resistance decreases our ability to treat infections, it is crucial to prevent infection through good hygiene and the appropriate use of biocides. More...
8.1 What factors increase the risk of resistance to both biocides and antibiotics?
Bacteria have the ability to transfer genes not only to their offspring but also from one organism to another, be it a similar bacterium or a different bacterial species. This horizontal transfer of DNA plays a very important role in the spread of bacterial resistance. The transfer is most effective between bacteria sharing the same ecological niche. Bacteria can be classified according to their efficiency at transferring genes. Some bacteria have developed highly specialised mechanisms to transfer genes and there is a high risk that they will pass genetic material to unrelated species. Medium-risk bacteria can only pass DNA to related species and low-risk bacteria are those with no known mechanism of transferring DNA to other organisms.
The presence of biocides can lead to the expression of a number of genes in bacteria that enable them to develop general defence mechanisms. These, in turn, can increase the bacteria’s resistance to antibiotics.
The risk of bringing about resistance also depends on the type of biocide used. Bacteria are unlikely to escape damage from highly reactive biocides so these do not readily lead to resistance unless they are used or stored incorrectly. Other biocides such as metallic salts and quaternary ammonium compounds are more prone to induce resistance because of the way they interact with bacteria. For many biocides used heavily in consumer products and in the food industry, there is little information on whether or not they can lead to resistance.
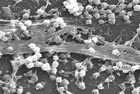
Growing as a community attached to a surface (biofilm) allows bacteria to survive under hostile conditions. Therefore, any circumstances that allow the formation of biofilms are a potential risk for developing resistance to both antibiotics and biocides. These include solid surfaces in the body such as prosthetics, catheters or implants, as well as surfaces in food and chemical factories, or in water treatment plants.
In water, environmental factors such as pH, the amount of oxygen and nutrients available, temperature and exposure time influence how bacteria grow and thus affect the way they respond and, sometimes, adapt to biocides. They also have an effect on how bacteria relate to other bacteria by transferring genetic mobile elements or by arranging themselves into biofilms. Large colonies of bacteria can act as one and activate resistance genes simultaneously by exchanging signal molecules. Environmental factors can affect this mechanism and therefore play a role in the development of resistance.
The large and indiscriminate use of biocides will increase the selection and dissemination of resistance genes among bacteria. As biocides used in homes and in industries come into contact with micro-organisms in animals and soil, they can lead to the emergence of resistance genes and the transfer of these between micro-organisms, including those in food. Therefore there is a risk that humans may be exposed to resistant bacteria through food, and this may concern a significant part of the population. More...
8.2 What (new) methods are required to effectively assess the risk of resistance?
There are no standard, internationally agreed methods of establishing the efficacy of biocides. Current tests vary from basic preliminary studies to sophisticated methods that aim to simulate the conditions found in practice.
Designing tests is complicated because many different factors have to be controlled. Results are often not reproducible, especially if the tests are carried out in real conditions outside the laboratory. Then again, tests in the laboratory can be too rigid, time-consuming and not represent the real conditions found in practice.
Samples of bacteria are often tested separately for resistance to antibiotics and to biocides but there are no set methods to determine resistance to both at the same time. The information available on the effectiveness of different biocides is inconsistent because of the wide range of testing methods used and because tests are not always carried out properly. There is an urgent need to design a standard method of measuring both biocide and antibiotic resistance in bacterial samples.
Bacteria are often present in the environment as biofilms and these play an important role in bacterial resistance. Despite this, most laboratories do not measure the efficacy of biocides on biofilms and there are no European standards for such tests. This is an important shortcoming because biofilms are ever-present and notoriously difficult to remove, even after intense cleaning. Moreover, higher concentrations of a biocide will most probably have to be used to clear biofilms and this will increase the amounts of biocide released to the environment.
The presence of biocides in the environment also increases the likelihood of developing resistance, especially when the concentrations are too low to be effective. Two specific situations need particular consideration: biocides that can persist in the environment for a long time, and biocides used or released frequently in places where there are many micro-organisms. More...
The Three-Level Structure used to communicate this SCENIHR Opinion is copyrighted by GreenFacts asbl/vzw.