1.1. Contact organisation
Ministère de la Santé et de la Sécurité sociale - Direction de la santé
1.2. Contact organisation unit
Pôle support à l'innovation - Service épidémiologie et statistique
1.3. Contact name
Confidential because of GDPR
1.4. Contact person function
Confidential because of GDPR
1.5. Contact mail address
Direction de la santé
20, rue de Bitbourg
L-1273 Luxembourg
Luxembourg
1.6. Contact email address
Confidential because of GDPR
1.7. Contact phone number
Confidential because of GDPR
1.8. Contact fax number
Confidential because of GDPR
2.1. Metadata last certified
27 May 2025
2.2. Metadata last posted
27 May 2025
2.3. Metadata last update
27 May 2025
3.1. Data description
Data on causes of death (CoD) provide information on mortality patterns and form a major element of public health information.
CoD data refer to the underlying cause which - according to the World Health Organisation (WHO) - is "the disease or injury which initiated the train of morbid events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury".
CoD data are derived from death certificates. In Luxembourg, certifier must be a physician (forensic or not) as define by the following legal basis: Grand-Ducal Regulation of 20 May 2020 amending the Grand-Ducal Regulation, as amended of 20 June 1963, making the declaration of causes of death compulsory.
The information provided in the medical certificate of cause of death is mapped to the International Statistical Classification of Diseases and Related Health Problems (ICD).
In Luxembourg, there is only one NUTS level : NUTS 0 = NUTS 1 = NUTS 2.
3.2. Classification system
Eurostat's CoD statistics build on standards set out by the World Health Organisation (WHO) in the International Statistical Classification of Diseases and Related Health Problems (ICD).
The regional breakdown is based on the Nomenclature of Territorial Units for Statistics (NUTS 2).
Classification and updates applied by years
| Data year | ICD classification used (ICD-9, ICD-10) (3 or 4 chars) | For ICD-10: updates used |
|---|---|---|
| 2011 | ICD-10 | STYX - updates of 2003 IRIS - updates of 2011 manual coding - updates of 2011 |
| 2012 | ICD-10 | ACS - updates of 2011 manual coding - updates of 2011 |
| 2013 | ICD-10 | ACS - updates of 2013 manual coding - updates of 2013 |
| 2014 | ICD-10 | ACS - updates of 2013 manual coding - updates of 2013 |
| 2015 | ICD-10 | ACS - updates of 2015 manual coding - updates of 2013 |
| 2016 | ICD-10 | ACS - updates of 2015 manual coding - updates of 2013 |
| 2017 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2018 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2019 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2020 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2021 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2022 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
| 2023 | ICD-10 | ACS - updates of 2016 manual coding - updates of 2016 |
3.3. Coverage - sector
Public Health
3.4. Statistical concepts and definitions
Concepts and definitions are described in the Commission regulation (EU) No 328/2011 in articles 2 and 3.
3.4.1. National definition used for usual residency
Place of residence declared by the civil register officer on the death certificate
3.4.2. Stillbirth definition and characteristics collected
a) National definition used for stillbirths
Until 2020, national recommendation of Health Ministry based on WHO definition : fetal death is death prior to the complete expulsion or extraction from its mother of a product of conception, when stillbirth is at least 500 gr birth weight or 22 weeks of gestational age; the death is indicated by the fact that after such separation the fetus does not breathe or show any other evidence of life, such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles.
Legal framework changed in 2020. The legal text precise that fetal-nenotal death certificate has to be used for declaration of all deaths of children before the 28th day of life and for all stillbirths that meet one of the following criteria:
- birth weight ≥ 500 grams or
- gestational age ≥ 22 completed weeks of gestation or
- height from crown to heel ≥ 25 centimeters.
b) What are the collected characteristics ?
Gestational age and birthweight
3.5. Statistical unit
The statistical units are the deceased persons and the stillborns, respectively, under condition that death occured on the national territory
3.6. Statistical population
By law, COD statistics covers all death cases occured on national territory (place of occurrence LU); as such they are considered by health authorities as “de facto” death case in Luxembourg.
3.6.1. Neonates of non-resident mothers
If neonates die on national territory (place of occurrence LU), they are considered by health authorities as “de facto” death case in Luxembourg.
Place of death is not a criteria defining place of residence.
Neonates of non-resident mothers are not considered as residents, even if they die on national territory (place of occurence LU).
3.6.2. Non-residents
By law, all death case occuring on the national territory (place of occurrence LU) has to be documented by a death certificate, regardless of the place of residence of the deceased person.
All non-residents dying on the national territory are covered by health authorities in the national death register as “de facto” death case.
3.6.3. Residents dying abroad
None of the residents dying abroad are covered by health authorities in the national death register as “de facto” death case.
Demographic death registry ("de juro" death case) collects administrative information on residents dying abroad but receive no medical information such as causes of death (natural neither external causes of death) concerning those residents dying abroad.
3.7. Reference area
Grand Duchy of Luxembourg.
Grand Duchy of Luxembourg has no regional or other subnational NUTS division of national territory: NUTS 0 = NUTS 1 = NUTS 2.
3.8. Coverage - Time
Eurostat time series are available from 1994 onwards.
Luxembourg times series are available since 1967 onwards.
3.9. Base period
Not applicable.
The unit is number.
Last reference period is 2023
6.1. Institutional Mandate - legal acts and other agreements
On national level, CoD data collection is legally defined in the Règlement grand-ducal du 20 mai 2020 modifiant le règlement grand-ducal modifié du 20 juin 1963 rendant obligatoire la déclaration des causes de décès.
This legal framework was modified in 2022 by the Règlement grand-ducal du 6 mai 2022 modifiant ... le règlement grand-ducal modifié du 20 juin 1963 rendant obligatoire la déclaration des causes de décès. Modifications do not impact the COD data collection (no modificiation of the medical part of the death certificate).
Luxembourg CoD microdata transmitted to WHO according to the Nomenclature Regulations from 1967.
Until reference year 2010, CoD data was submitted to Eurostat on the basis of a gentleman's agreement established in the framework Eurostat's Working Group on "Public Health Statistics".
A Regulation on Community statistics on public health and health and safety at work (EC) No 1338/2008 was signed by the European Parliament and the Council on 16 December 2008. This Regulation is the framework of the data collection on the domain.
Within the context of this framework Regulation, a Regulation on Community statistics on public health and health and safety at work, as regards statistics on causes of death (EU) No 328/2011 was signed by the European Parliament and the Council on 5 April 2011.
Luxembourg CoD microdata according to this regulation is submitted to Eurostat since reference year 2011.
6.2. Institutional Mandate - data sharing
National COD data are shared with:
- Eurostat according to the Regulation No 328/2011 (microdata)
- WHO World (agregated data shared on basis of the Nomenclature Regulations from 1967)
- National statistical office STATEC (agregated data) according to article 13 of Loi du 10 juillet 2011 portant organisation de l'Institut national de la statistique et des études économiques et modifiant la loi modifiée du 22 juin 1963 fixant le régime des traitements des fonctionnaires de l'Etat.
- National Cancer Registry of Luxembourg (microdata) according to article 5 of Règlement grand-ducal du 18 avril 2013 déterminant les modalités et conditions de fonctionnement du registre national du cancer et modifiant le règlement grand-ducal du 20 juin 1963 rendant obligatoire la déclaration des causes de décès.
7.1. Confidentiality - policy
Regulation (EC) No 223/2009 on European statistics (recital 24 and Article 20(4)) of 11 March 2009 (OJ L 87, p. 164), stipulates the need to establish common principles and guidelines ensuring the confidentiality of data used for the production of European statistics and the access to those confidential data with due account for technical developments and the requirements of users in a democratic society.
7.2. Confidentiality - data treatment
The GDPR (EU) 2016/679 of the European Parliament and of the Council of 27th of April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data precise in his “whereas (27)” it does not apply to the personal data of deceased persons. Member States may provide for rules regarding the processing of personal data of deceased persons.
However, some specific treatment rules are historically applied and maintained since GDPR came into force in 2018.
No microdata is published.
Only aggregated data is published with a granularity level based on :
- 5-years-agegroups,
- Sex and
- ICD-10 codes with 3 digits.
8.1. Release calendar
Once quality control on national data is finished before ending of the 24 months time laps defined in the Regulation on Community statistics on public health and health and safety at work, as regards statistics on causes of death (EU) No 328/2011, COD yearbook is published with a press release.
Once this is done:
- Yearbook is sent to all authorized practicing physician in Luxembourg
- Microdata are prepared for and sent to Eurostat and National Cancer Registry
- Agregated data are prepared for and sent to WHO and STATEC (National Statistical Office)
8.2. Release calendar access
Not applicable.
8.3. Release policy - user access
Once COD yearbook press release is published, it is freely available and downloadable on:
Annual
10.1. Dissemination format - News release
News releases online.
10.2. Dissemination format - Publications
Causes of death yearbook (Statistiques des causes de décès pour l’année YYYY) disseminated in dashboards and PDF format on the National Health Portal.
10.3. Dissemination format - online database
Institut national de la statistique et des études économiques du Grand-Duché du Luxembourg (STATEC)
10.3.1. Data tables - consultations
Not available
10.4. Dissemination format - microdata access
All access to COD microdata has to be formally requested adressing the Director of the Directorate of Health. The Director is the only one who can allow this access.
By law, microdata are transmitted to the National Cancer Registry: Règlement grand-ducal du 18 avril 2013 déterminant les modalités et conditions de fonctionnement du registre national du cancer (see article 5, section 2).
10.5. Dissemination format - other
Aggregated data disseminated online (MSexcel and PDF) and in a hard copy paper yearbook.
PDF document: Causes of death yearbook (Statistiques des causes de décès pour l’année YYYY) disseminated on the National Health Portal.
MSexcel files disseminated on National Statistics Portal.
10.5.1. Metadata - consultations
Not available
10.6. Documentation on methodology
Mortality in Luxembourg: historical developments, current situation and future prospects of the national mortality monitoring system (only in French)
La mortalité au Luxembourg: évolution historique, situation actuelle et perspectives futures du système national de surveillance de la mortalité
Causes of death yearbook (Statistiques des causes de décès pour l’année YYYY) disseminated in PDF format on the National Health Portal.
10.6.1. Metadata completeness - rate
100% of
- All doctors (certifiers) trained in the certification
- Certificates filled by persons who attented a course on certification fo post-mortem examination (autopsies)
Following indicators are not yet measurable :
- All doctors (certifiers - pathologists or others doctors) trained in the post-mortem examination (autopsies)
- Death certificates that are queried (only queries related to medical part of the death certificate should be included)
- Replies received for queries sent
- Deaths where the underlying cause is changed as a result of the query
- Death certificates with incorrect sequence
10.7. Quality management - documentation
2023 : Development of an R script to produce datasets to be sent to National Statistical Office
2022 : Development of an R script to produce datasets to be sent to EUROSTAT and WHO
2022: Since the introduction at 1st of August 2021 of two new COD forms (one for fetal and neonatal deaths and another for all other deaths), development of a new adapted database (internal document, in development).
2021: Development of an R script tested and validated on 2020 COD dataset (internal document).
2021: Development of an QlikSense script automatizing generation of all tables of the annual COD yearbook (internal document).
2021: Written procedure describing the coding and data entry of death certificates into the national register of causes of death in Luxembourg (internal document).
2021: Development of an R script automatizing quality control on yearly COD dataset (internal document).
2021: Development of an R script automatizing production of quality control indicators from 1998 till nowadays
- For all deaths of residents occurring on the national territory: measurement of the completeness of the register by comparing
- De facto deaths: register of causes of death (non-residents deceased in Lux IN - residents deceased abroad OUT)
- De jure deaths: national register of natural persons (non-residents deceased in Lux OUT - residents deceased abroad IN)
- For all deaths occurring on the national territory
- Evolution from 1998 till nowadays published in annual yearbook
- Symptoms, signs and abnormal results of clinical and laboratory examinations, nca (# of R00 to R99 and % of A00-Y98)
- Unwitnessed deaths and other ill-defined and unspecified causes of death (# of R98 and R99 and % of A00-Y98)
- Senility (# of R54 and % of A00-Y98)
- Exposure to factors, unspecified (# of X59 and % of A00-Y98)
- WHO ill-defined deaths (# of R00-R94, R96-R99, Y10-Y34, Y87.2, C76, C80, C97, I47.2, I49.0, I46, I50, I51.4, I51.5, I51.6, I51.9, I70.9 and % of A00-Y98)
- 4-digit codes with a 4th digit ".8" ... "other" (# of ".8" and § of 4-digit codes)
- 4-digit codes with a 4th digit ".9" ... "unspecified" (# of ".9" and % of 4-digit codes)
- Evolution from 1998 till nowadays published in annual yearbook
- Number and proportion of deaths occurring in a health care setting (hospital, maternity, nursing or elderly home)
- For deaths occurring in hospital
- Symptoms, signs and abnormal results of clinical and laboratory examinations, nca (# of R00 to R99 and % of A00-Y98)
- Unwitnessed deaths and other ill-defined and unspecified causes of death (# of R98 and R99 and % of A00-Y98)
- Senility (# of R54 and % of A00-Y98)
- Exposure to factors, unspecified (# of X59 and % of A00-Y98)
- WHO ill-defined deaths (# of R00-R94, R96-R99, Y10-Y34, Y87.2, C76, C80, C97, I47.2, I49.0, I46, I50, I51.4, I51.5, I51.6, I51.9, I70.9 and % of A00-Y98)
- 4-digit codes with a 4th digit ".8" ... "other" (# of ".8" and % of 4-digit codes)
- 4-digit codes with a 4th digit ".9" ... "unspecified" (%# of ".9" and % of 4-digit codes)
- Autopsies
- Number of deaths certified by a doctor "authorised to perform autopsies" (# of these deaths certified by a forensic doctor and % of A00-Y98)
- Number of hospital deaths certified by a doctor "authorised to perform autopsies" (# of these hospital deaths certified by a forensic doctor and % of A00-Y98)
- Comparison with figures published by the national Forensic Medicine Department
- Number of forensic medical autopsies
- Number of forensic autopsies
- Total number of autopsies (# of autopsies and % of A00-Y98)
2012: Impact of methodological changes in the automatic coding system (Styx versus Iris) of causes of death on mortality statistics in Luxembourg. 100% of the 2,296 death certificates collected from January 2011 to July 2011, routinely coded by the coder with the help of the French Styx software, were coded twice with the Iris software. The results of the two automatic coding systems were then compared: on the one hand, the number of deaths by ICD-10 codes coded with Styx and on the other hand, the number of deaths by ICD-10 codes coded with Iris. The ratio and the absolute difference measure the differences in results between these two automatic coding tools, as well as the impact in figures that this methodological change will have had on the statistical data of subsequent years. (Internal study whose main first results were presented at the IRIS user group meeting in Köln (Germany) in September 2012.
11.1. Quality assurance
The causes of death data are based on a regulation, which defines scope, definitions of variables and characteristics of the data.
11.2. Quality management - assessment
A quality assessment of Eurostat's COD statistics was organised in May and June 2008. In that framework, a questionnaire was sent to Eurostat's partners (data providers) for COD statistics and a user survey was set up on Eurostat's website, for which 25 partners and 34 users answered. A questionnaire was also filled in by responsible people of COD statistics in Eurostat.
After verifying completeness of annual causes of death statistics, a formalized “quality control process” is launched considering different reference documents such as :
- OMS, 2008, « Classification statistique internationale des maladies et des problèmes de santé connexes », 10ième révision, édition 2008, 2ième volume Ed. OMS.
- WHO, 2013, « Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme - WHO Ausgabe », 10. Revision, Version 2013, Band 2 Regelwerke, WHO Ausgabe.
- Pace Asiak R., Bonte J., Kardaun J., Leitner B., Selb J., Gagel S., Niederlaender E., 2007, « European Statistics on Causes of Death - COD - Methodological information on implementation of the recommendations of the ad-hoc Task Force on Quality Control », Ed. Eurostat.
- Few specific additional elements of this “quality control” procedure are also launched every year.
12.1. Relevance - User Needs
Important international stakeholders
- WHO World: specific causes of death statistics
- WHO Euro: microdata for every single reference year, mortality indicators in Health for all database
- Unicef: electronic Joint Reporting on communicable diseases including some causes of deaths due to those communicable diseases
- EU Commission: specific causes of death statistics
- OECD: specific causes of death statistics for Health at a Glance, Country profile, etc.
- International agencies: EMCDDA, EuroMOMO, ECDC, etc.
Important national stakeholders
- Parliament: contributions in answers to parliamentary questions, public health thematic parliament debates
- Public administrations such as ministries, agencies: Road traffic accidents Commission of Transport Ministry preparing consolidated statistic
Important national researchers
- University of Luxembourg: National Youth Report
- Luxembourg Institute of Health: causes of death microdata for National Cancer Registry
Students (such as medicine students, health professions and public health professionals) requiring data/indicator for master or PhD thesis.
Media, civil society and citizens interested in specific causes of death statistics when “health related international days” have to be statistically documented.
12.2. Relevance - User Satisfaction
Not available
12.3. Completeness
National law defines:
- Those variables collected in both LU death certificates (fetal and neonatal death certificate, general death certificate)
- That causes of death are coded using WHO ICD nomenclature (Grand-Ducal Regulation of 20 June 1963 making the declaration of causes of death compulsory).
European law defines:
- The full list of variables that all member state has to transmit to Eurostat (Commission Regulation (EU) No 328/2011 of 5 April 2011 implementing Regulation (EC) No 1338/2008 of the European Parliament and of the Council on Community statistics on public health and health and safety at work, as regards statistics on causes of death Text with EEA relevance)
National COD data collection enables LU to send all required data to Eurostat.
12.3.1. Data completeness - rate
1. For mandatory variables:
100%
2. For voluntary variables:
100% except age of mother and parity that are collected in the new COD certificat only since 1st of August 2021.
New fetal-neonatal death certificate voted by law in May 2020 but, because of COVID crisis, disseminated for used form 1st of August 2021, specifically collect those variables (age of mother and parity).
3. For additional variables:
- External CoD
100%
- Place of occurrence for external CoD
100%
- Activity for external CoD
0%
New death certificate voted by law in May 2020 but, because of COVID crisis, disseminated for used form 1st of August 2021, specifically collect these variable.
13.1. Accuracy - overall
High accuracy for death occured in Luxembourg, legal obligation to provide a death certificate for every death occurrin the national territory of Luxembourg.
Lack of information concerning causes of deaths by young resident children and adolescents aged between 5 and 14 years. Part of those deaths concern kids suffering a serious illness and therefore transferred in specialised health centres in neighbour countries. In case those children die abroad, Luxembourg health authority are not informed of the death case nor the causes of death.
13.2. Sampling error
Not applicable. Data collection is from administrative sources.
13.2.1. Sampling error - indicators
Not applicable.
13.3. Non-sampling error
Errors related with :
- Data collection: no errors documented.
- Measurement: important part of children and adolescent residents die abroad so that civil register is aware of those “de juro” death cases but causes of death register is not aware (those death cases are not “de facto death cases”) :
- Between 1994 and 2007, one third to one half of all 1 to 14-years-old died aboard (Mortality in Luxembourg: historical developments, current situation and future prospects of the national mortality monitoring system - only in French).
- Mortality statistics of 1 to 14-years-old have to be interpreted with caution.
- Processing: no errors documented.
- Coding: no errors documented.
13.3.1. Coverage error
Not applicable.
13.3.1.1. Over-coverage - rate
Residents dying abroad are not reported in LU national COD statistics.
Non-residents dying in LU are reported in LU national COD statistics.
13.3.1.2. Common units - proportion
Not applicable.
All COD data are collected via a unique national administrative source:
- a fetal and neonatal death certificate.
- a general death certificate.
13.3.2. Measurement error
Not applicable.
13.3.3. Non response error
Not applicable.
13.3.3.1. Unit non-response - rate
Not applicable.
13.3.3.2. Item non-response - rate
Not applicable.
13.3.4. Processing error
Not applicable.
13.3.5. Model assumption error
Not applicable.
14.1. Timeliness
| Year | Number of months between the end of the reference year and the publication at national level |
|---|---|
| 2011 | 11 |
| 2012 | 10 |
| 2013 | 11 |
| 2014 | 23 |
| 2015 | 14 |
| 2016 | 17 |
| 2017 | 23 |
| 2018 | 22 |
| 2019 | 16 |
| 2020 | 23 |
| 2021 | 13 |
| 2022 | 11 |
| 2023 | 13 |
14.1.1. Time lag - first result
Not applicable.
14.1.2. Time lag - final result
Not applicable.
14.2. Punctuality
From data collection with reference year 2011 onwards, Eurostat asks for the submission of final data at national and regional level and related metadata for the year N at N+24 months, according to the Implementing Regulation (EC) No. 328/2011, Article 4.
14.2.1. Punctuality - delivery and publication
| Reference year | Time between the end of the reference year and the delivery of final data to Eurostat |
|---|---|
| 2011 | 11 |
| 2012 | 10 |
| 2013 | 11 |
| 2014 | 23 |
| 2015 | 14 |
| 2016 | 17 |
| 2017 | 23 |
| 2018 | 22 |
| 2019 | 16 |
| 2020 | 23 |
| 2021 | 13 |
| 2022 | 11 |
| 2023 | 13 |
15.1. Comparability - geographical
In Luxembourg, there is no subnational level of collecting, coding, transmiting COD data.
In Luxembourg, NUTS 0 = NUTS 1 = NUTS 2.
15.1.1. Asymmetry for mirror flow statistics - coefficient
Not applicable.
15.2. Comparability - over time
Coding procedures changed over time in Luxembourg :
- ICD versions :
- ICD7 from 1967 to 1970
- ICD8 from 1971 to 1978
- ICD9 from 1979 to 1997
- ICD10 from 1998 until nowadays
- automatic coding systems :
- STYX from 2004 to July 2011
- IRIS from January 2011 until nowadays
15.2.1. Length of comparable time series
Considering evolution of ICD versions in use (ICD7 until 1970, ICD8 until 1978, ICD9 until 1997 and ICD10 since 1998) and automatic coding systems in use (Styx from 2004 until July 2011 and IRIS since January 2011), the number of reference periods since last break is 10 periods (from 2011 until 2020).
15.3. Coherence - cross domain
For death cases ocurred in the country, coverage is estimated complete (100%).
Residents dying abroad are not included in national statistics, there is an important lack of coverage for 5 to 14 years-old children (about one third of this age group who died between 1994 and 2007 died abroad).
Coherence of residents dying in the country between data available from demography ("de juro" death cases) and data available from COD ("de facto" death cases) is monitored every year and published in the national COD yearbook:
- From 1994 until 2016, around 1% of resident death cases in Luxembourg were more exhaustively documented in the causes of death registry ("de facto" death cases) than in the demographic registry ("de juro" death cases).
- Since 2017, demographic registry has improved his data collection and collect around 0.4% more resident death cases in Luxembourg than the causes of death registry.
For more information :
- Mortality in Luxembourg: historical developments, current situation and future prospects of the national mortality monitoring system - only in French
- Statistics on causes of death
15.3.1. Coherence - sub annual and annual statistics
Not applicable, only annual data are available.
15.3.2. Coherence - National Accounts
Not applicable.
15.4. Coherence - internal
The data are consistent within a given data set.
The cost and burden of the data collection is reduced by using validation and dissemination IT tools. Costs per year are estimated as following:
Costs related to data collection
- Print cost of around 4000 death certificates: 3 000,00€
- Per post sending of around 4000 filled death certificates: 1 000,00€
Costs related to data codification
- Luxembourg actively contributes since many years to Iris Institute activities and paying since 2020 annual fees for Iris support model 2: 10 000,00 €
Costs related to data dissemination
- Dissemination of paper hard copies has been drastically reduced in 2020 giving priority of electronic dissemination of PDF files: 0,00 €
- About 100 hard copies of annual COD yearbook are send per post: 400,00 €
17.1. Data revision - policy
Not applicable.
17.2. Data revision - practice
There is no systematic revision of previous year data.
17.2.1. Data revision - average size
Not applicable.
18.1. Source data
Causes of death statistics are based on the information daily collected from the national death certificate (completed by the physician who certifies the death). Socio-demographic data is double-checked with the one collected in the national population register.
18.2. Frequency of data collection
Every day ongoing data collection and, once control quality checks are finalized on the completed annual datase, statistical analysis begins.
18.3. Data collection
Luxembourg has a general death certificate and since end of the 60s a specific perinatal death certificate which is mandatory for stillbirths and neonatal deaths till the 10th day of life. A specific perinatal death certificate is necessary to facilitate the collection of information on perinatal mortality, and to improve the quality of birth registers.
In May 2020, both models were update by law : the main change concerns application period of fetal-neonatal death certificate that has to be filled in during the whole neonatal period (early + late neonatal period) of the first 28 days of life. Because of COVID crisis, new forms could not be disseminated before July 2021 for first use from 1st of August 2021 on.
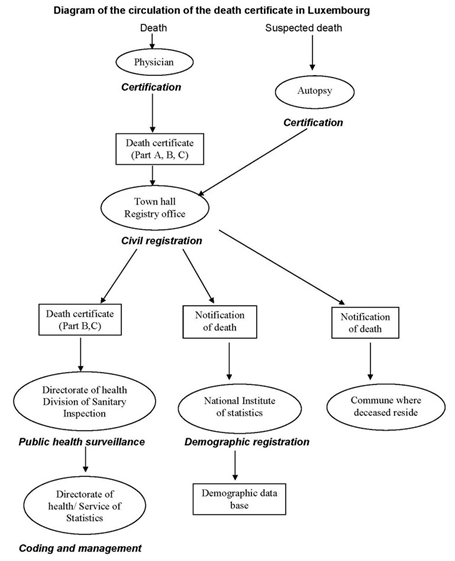
Both death certificates are divided into two administrative parts and one medical part.
- Part A : administrative part 1 remains in the civil register
- Part B : administrative part 2 is sent to health authorities
- Part C : medical part is sent to health authorities
Below the circulation of the death certificate is mapped:
For more information :Mortality in Luxembourg: historical developments, current situation and future prospects of the national mortality monitoring system - only in French
18.3.1. Certification
Table on certification (Percentage)
| Year |
All doctors (certifiers) trained in the certification | All doctors (certifiers - pathologists or others doctors) trained in the post-mortem examination (autopsies) | Certificates filled by persons who attended a course on certification or post-mortem examination | Death certificates that are queried (only queries related to medical part of the death certificate should be included) | Replies received for queries sent | Deaths where the underlying cause is changed as a result of the query | Death certificates with incorrect sequence |
|---|---|---|---|---|---|---|---|
| 2011 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2012 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2013 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2014 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2015 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2016 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2017 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2018 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2019 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2020 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2021 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2022 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
| 2023 | 100% | not applicable | 100% | not applicable | not applicable | not applicable | not applicable |
18.3.2. Automated Coding
| Data year | Use of any form of automated coding | System used (IRIS, MICAR, ACME, STYX, MIKADO, others) |
|---|---|---|
| 2011 | Yes | STYX from 01-01-2011 to 31-07-2011 IRIS from 01-08-2011 to 31-12-2011 |
| 2012 | Yes | IRIS |
| 2013 | Yes | IRIS |
| 2014 | Yes | IRIS |
| 2015 | Yes | IRIS |
| 2016 | Yes | IRIS |
| 2017 | Yes | IRIS |
| 2018 | Yes | IRIS |
| 2019 | Yes | IRIS |
| 2020 | Yes | IRIS |
| 2021 | Yes | IRIS |
| 2022 | Yes | IRIS |
| 2023 | Yes | IRIS |
18.3.3. Underlying cause of death
| Data year | Only manual selection of underlying cause | Manual with ACME decision tables (if yes, version of ACME) | ACS utilising ACME decision tables (if yes, version of ACME) | Own system (ACS without ACME) | Comments |
|---|---|---|---|---|---|
| 2011 | IRIS with ACME | ||||
| 2012 | IRIS with ACME | ||||
| 2013 | IRIS v4.0.3 with ACME | ||||
| 2014 | IRIS v4.2.3 with ACME | ||||
| 2015 | IRIS v4.5.0 with ACME | ||||
| 2016 | IRIS v4.5.3 with ACME | ||||
| 2017 | IRIS v4.5.6 with ACME | ||||
| 2018 | IRIS v5.5.0 Y2018S1 | Downloads Iris Institute | |||
| 2019 | IRIS v5.6.0 | Downloads Iris Institute | |||
| 2020 | IRIS v5.7.0 | Downloads Iris Institute | |||
| 2021 | IRIS v5.8.0 | Downloads Iris Institute | |||
| 2022 | IRIS v5.8.1 | Downloads Iris Institute | |||
| 2023 | IRIS v6.0.17 | Downloads Iris Institute |
18.3.4. Availability of multiple cause
| Data year | Information stored in the national CoD database, UC (Underlying cause) or MC (Multiple cause) |
|---|---|
| 2011 | UC + MC 4 digits |
| 2012 | UC + MC 4 digits |
| 2013 | UC + MC 4 digits |
| 2014 | UC + MC 4 digits |
| 2015 | UC + MC 4 digits |
| 2016 | UC + MC 4 digits |
| 2017 | UC + MC 4 digits |
| 2018 | UC + MC 4 digits |
| 2019 | UC + MC 4 digits |
| 2020 | UC + MC 4 digits |
| 2021 | UC + MC 4 digits |
| 2022 | UC + MC 4 digits |
| 2023 | UC + MC 4 digits |
18.3.5. Stillbirths and Neonatal certificates
a) Stillbirths
Luxembourg has implemented since the end of the 60´ a specific perinatal death certificate, which is mandatory for stillbirths and neonatal deaths aged less than 10 days.
b) Neonates
Luxembourg has implemented since the end of the 60´ a specific perinatal death certificate, so early neonatal death cases (aged less than 10 days) are registered via this specific death certificate and late neonatal death cases are registered via the general death certificate.
Legal framework changed in 2020. The legal text and a new version of this specific fetal-neonatal death certificate is implemented from 1st of August 2021 onwards.
- The period covered by this new fetal-neonatal death certificate concerns death cases occured during the whole(early and late) neonatal period, until the 28th day of life.
- A fetal-nenotal death certificate has to be fill for :
- all deaths of children before the 28th day of life
- all stillbirths that meet one of the following criteria
- birth weight ≥ 500 grams or
- gestational age ≥ 22 completed weeks of gestation or
- height from vertex to heel ≥ 25 centimeters.
18.4. Data validation
- Consultations with national civil register led by national statistical office STATEC
- Consultations with national perinatal register called SUSANA-DIANE-PERINAT
- Yearly verifications for stillbirths and infant death cases
- Yearly verifications of residents dying in LU registered by COD register and by civil register:
- from 1994 until 2017, MoH had every year aroung 1 % more death cases of residents dying in Luxembourg than the national civil register
- from 2018, national civil register having improved is data collection, collects aroung 0.4 % more death cases of residents dying in Luxembourg than COD register
- Yearly verifications (automatic) of the Eurostat and WHO ICD-10 recommendations
18.4.1. Coding
Description of coding procedure (central level, distributed among other bodies, etc.):
Once administrative part (B) and medical part (C) of death certificate arrives in Directorate of health (central level), all transmitted information is coded in Epidemiology and statistics unit of Directorate of health by expert coders.
Description of the procedures to detect errors (i.e.errors such as potential inconsistency in the death certificate or error due to mistake when filling the deaths certificates):
Coding procedure define and describe error atomatic detection steps under condition that deceased was resident in Luxembourg:
- Check of consistency of the identity of deceased between death certificate and civil register
- Check of consistency of the vital status “dead” of deceased between death certificate and civil register
- Check of consistency of the date of death of deceased between death certificate and civil register
- Check of consistency between date of birth and national ID number
- Check of consistency of municipality of residence between death certificate and civil register
Description of the overall national quality procedure :
After verifying completeness of annual causes of death statistics, a formalized “quality control process” is launched considering different reference documents such as :
- OMS, 2008, « Classification statistique internationale des maladies et des problèmes de santé connexes », 10ième révision, édition 2008, 2ième volume Ed. OMS.
- WHO, 2013, « Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme - WHO Ausgabe », 10. Revision, Version 2013, Band 2 Regelwerke, WHO Ausgabe.
- Pace Asiak R., Bonte J., Kardaun J., Leitner B., Selb J., Gagel S., Niederlaender E., 2007, « European Statistics on Causes of Death - COD - Methodological information on implementation of the recommendations of the ad-hoc Task Force on Quality Control », Ed. Eurostat.
- Few specific additional elements of this “quality control” procedure are also launched every year.
International recommanded quality checks and national additional controls are performed :
- Check that :
- All death case has at least one cause of death (underlying cause of death)
- All death case due to external causes of death (as underlying cause of death) has also a S-T code (injury, poisoning and certain other consequences of external causes) in second position
- Check of potential inconsistencies for the following categories:
- Codes for conditions incapable of causing death
- Codes linked to gender
- Age related codes
- Codes not allowed as primary cause
- Codes to be reassigned
- Asterisk codes (related to dagger codes) not allowed as underlying causes of death
- Codes not to be used if the primary cause is known
- Double check of categories of sequelae
- Verification of the 4th digit of codes for external causes of death
- Check that complications of surgical and medical procedures are not used as the underlying cause
- Double check of ill-defined conditions
- Basic plausibility tests (consistency between date of birth and date of death, duplicates, check that sex is known)
- Double check of notifiable diseases
- Fetal mortality from unspecified cause
- Stillbirths and neonates with missing mandatory variables (birthweight and gestational age)
- Double check of autopsies
- Double check of covid-19 cases
- X20-X29 codes are double checked.
- P codes for deceased people aged more than 12 months are double checked.
- Stillbirths and infant death with an underlying cause of death other than a P or Q code are double checked.
- Kids dying under the age of 10 years dying from an external cause of death are double checked.
- Every V01 to Y98 cause of death has an attached S or T code.
- All C53, C54 and C55 date cases are double checked with national cancer registry to reduce C55 frequency (since entry in force of GDPR, this double check is not anymore possible).
- Since 2020, all U codes are double checked.
- Exhaustiveness of the registry is measured comparing number of residents dying in national territory documented by National Statistics Office (“de juro” definition) and those documented by Health Authorities (“de facto” definition)
- Calculation and monitoring before publication in the COD yearbook of a set of quality indicators (anywhere / hospital):
- R00 to R99
- R54
- R98 and R99
- X59
- WHO ill-defined deaths: R00-R94, R96-R99, Y10-Y34, Y87.2, C76, C80, C97, I47.2, I49.0, I46, I50, I51.4, I51.5, I51.6, I51.9, I70.9
- .8 and .9 as 4th digit
- Number of death causes certified by forensic physicians
- Distribution of manually versus automatically coded underlying causes of death
Description of the measures taken in order to solve detected errors:
In case of inconsistency, interaction with local and/or civil register to understand and correct errors concerning:
- Identity of deceased
- Date of birth
- Date of death
- Municipality of residence
In case of inconsistency between sex and ICD10 codes, errors are deleted and substituted by correct data.
Coding performed by a certifier:
By law, all certifiers have to be medical doctor or forensic doctor.
According to WHO ICD recommendations, certifiers are required to communicate causes of death in text format. ICD10 codes are not recommended by WHO to be used by certifiers to communicate causes of death.
Coders are specifically and continuously trained in ICD10 coding and use of IRIS automatic coding system.
Coders interact with certifiers in case written causes of death are not readable or are incomplete.
Estimation of the percentage of autopsy from which information is available for coding:
In Luxembourg, coexists two kind of autopsies: medico-legal autopsy and medical autopsy for scientific purposes:
- 100 % of medico-legal autopsy produce information that is available substituting the initial death certificate produced by a first certifier with a new death certificate produced by coroner. From 1st of August 2021, with the use of the new death certificate, in case of a medico-legal autopsy, conorer will complete the initial death certificate produced by the first certifier.
- Until 2018, most of the medical autopsy for scientific purposes (over 90%) produce information that were used for enriching medical part of death certificate to better precise causes of death and ICD10 codes. Since the entry in force of GDPR in May 2020, causes of death registry has no more access to those medical autopsies.
Description of double coding exercises and rate of codification errors for underlying cause of death:
Luxembourg registry of causes of death uses since 2004 an automatic coding system reducing manual coding of causes of death and manual identification of the underlying cause of death:
- STYX from 2004 to July 2011
- IRIS from January 2011 until nowadays
In 2020, 95.1% of all underlying causes of deaths were automatically coded with IRIS and selected among all multiple causes of death (maximum of 6 causes) certified by the certifier.
For reducing errors in typing of codes, all codified variable are recorded twice:
- First step, all codified administrative data (part B of death certificate) of all death certificates are recorded in the national database.
- Second step, all codified medical data (part C of death certificate) of all death certificates are recorded in the national database.
- Third step, all codified administrative and medical data (part B and part C of death certificate) of all death certificates are double-recorded in the national database. Every inconsistency between initial-record and double-record is warned by a pop-up window requiring the correction of the wrongly recorded data before definitive record of the death case in the national database.
The full description of the quality controls implemented can be found in the document "Quality control procedures of causes of death" given in annex.
Annexes:
Quality control procedures of causes of death
18.4.2. Unspecified CoD code
ICD codes for the underlying cause (% of the Total)
| Year | Unspecified CoD (for ICD10: R00-R99 codes, for ICD9: 780-790 codes) | Unknown CoD (for ICD10: R98-R99 codes, for ICD9: 799.9, 798.9, 798.2 codes) | Deaths due to senility (for ICD10: R54 code, for ICD9: 797 code) | Deaths due to exposure to unspecified factor (for ICD10: X59 code, ICD9: 928.9 code) | WHO Ill-defined codes (for ICD10: R00-R94, R96-R99, Y10-Y34, Y87.2, C76, C80, C97, I47.2, I49.0, I46, I50, I51.4, I51.5, I51.6, I51.9, I70.9) |
|---|---|---|---|---|---|
| 2011 | 3,0% | 0,7% | 0,4% | 0,9% | 14,2% |
| 2012 | 2,9% | 0,5% | 0,4% | 0,8% | 13,0% |
| 2013 | 2,7% | 0,6% | 0,7% | 1,1% | 11,6% |
| 2014 | 2,5% | 0,6% | 0,5% | 0,9% | 12,0% |
| 2015 | 3,1% | 0,7% | 0,6% | 0,8% | 12,0% |
| 2016 | 3,1% | 0,6% | 0,7% | 1,2% | 12,3% |
| 2017 | 3,4% | 0,7% | 1,0% | 0,6% | 12,0% |
| 2018 | 2,8% | 0,6% | 0,5% | 1,1% | 10,9% |
| 2019 | 4,3% | 1,4% | 0,6% | 0,8% | 12,5% |
| 2020 | 3,6% | 1,4% | 0,6% | 0,6% | 9,6% |
| 2021 | 4,1% | 1,8% | 0,6% | 0,9% | 10,3% |
| 2022 | 4,2% | 1,9% | 0,6% | 0,7% | 10,9% |
| 2023 | 4,6% | 1,6% | 0,8% | 1,0% | 11,9% |
18.4.3. Unknown country or region
Unknown country/region (%) for residents and non-residents who died in the country
| Year | Residents | Non-residents | |||
|---|---|---|---|---|---|
| Unknown residency (NUTS2) | Unknown occurrence (NUTS2) | Unknown residency (country) | Unknown residency (NUTS2) | Unknown occurrence (NUTS2) | |
| 2011 | 0,0% | 0,0% | 21,0% | 98,0% | 0,0% |
| 2012 | 0,0% | 0,0% | 16,0% | 99,0% | 0,0% |
| 2013 | 0,0% | 0,0% | 12,0% | 66,0% | 0,0% |
| 2014 | 0,0% | 0,0% | 5,0% | 43,0% | 0,0% |
| 2015 | 0,0% | 0,0% | 8,0% | 34,0% | 0,0% |
| 2016 | 0,0% | 0,0% | 7,0% | 23,0% | 0,0% |
| 2017 | 0,0% | 0,0% | 8,0% | 19,0% | 0,0% |
| 2018 | 0,0% | 0,0% | 8,0% | 25,0% | 0,0% |
| 2019 | 0,0% | 0,0% | 4,0% | 25,0% | 0,0% |
| 2020 | 0,0% | 0,0% | 4,0% | 24,0% | 0,0% |
| 2021 | 0,0% | 0,0% | 4,0% | 22,0% | 0,0% |
| 2022 | 0,0% | 0,0% | 7,0% | 22,0% | 0,0% |
| 2023 | 0,0% | 0,0% | 6,0% | 23,0% | 0,0% |
18.4.4. Validation of the coverage
Not applicable.
18.5. Data compilation
Not applicable.
18.5.1. Imputation - rate
Not applicable.
18.6. Adjustment
Not applicable.
18.6.1. Seasonal adjustment
Not applicable.
Data on causes of death (CoD) provide information on mortality patterns and form a major element of public health information.
CoD data refer to the underlying cause which - according to the World Health Organisation (WHO) - is "the disease or injury which initiated the train of morbid events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury".
CoD data are derived from death certificates. In Luxembourg, certifier must be a physician (forensic or not) as define by the following legal basis: Grand-Ducal Regulation of 20 May 2020 amending the Grand-Ducal Regulation, as amended of 20 June 1963, making the declaration of causes of death compulsory.
The information provided in the medical certificate of cause of death is mapped to the International Statistical Classification of Diseases and Related Health Problems (ICD).
In Luxembourg, there is only one NUTS level : NUTS 0 = NUTS 1 = NUTS 2.
27 May 2025
Concepts and definitions are described in the Commission regulation (EU) No 328/2011 in articles 2 and 3.
The statistical units are the deceased persons and the stillborns, respectively, under condition that death occured on the national territory
By law, COD statistics covers all death cases occured on national territory (place of occurrence LU); as such they are considered by health authorities as “de facto” death case in Luxembourg.
Grand Duchy of Luxembourg.
Grand Duchy of Luxembourg has no regional or other subnational NUTS division of national territory: NUTS 0 = NUTS 1 = NUTS 2.
Last reference period is 2023
High accuracy for death occured in Luxembourg, legal obligation to provide a death certificate for every death occurrin the national territory of Luxembourg.
Lack of information concerning causes of deaths by young resident children and adolescents aged between 5 and 14 years. Part of those deaths concern kids suffering a serious illness and therefore transferred in specialised health centres in neighbour countries. In case those children die abroad, Luxembourg health authority are not informed of the death case nor the causes of death.
The unit is number.
Not applicable.
Causes of death statistics are based on the information daily collected from the national death certificate (completed by the physician who certifies the death). Socio-demographic data is double-checked with the one collected in the national population register.
Annual
| Year | Number of months between the end of the reference year and the publication at national level |
|---|---|
| 2011 | 11 |
| 2012 | 10 |
| 2013 | 11 |
| 2014 | 23 |
| 2015 | 14 |
| 2016 | 17 |
| 2017 | 23 |
| 2018 | 22 |
| 2019 | 16 |
| 2020 | 23 |
| 2021 | 13 |
| 2022 | 11 |
| 2023 | 13 |
In Luxembourg, there is no subnational level of collecting, coding, transmiting COD data.
In Luxembourg, NUTS 0 = NUTS 1 = NUTS 2.
Coding procedures changed over time in Luxembourg :
- ICD versions :
- ICD7 from 1967 to 1970
- ICD8 from 1971 to 1978
- ICD9 from 1979 to 1997
- ICD10 from 1998 until nowadays
- automatic coding systems :
- STYX from 2004 to July 2011
- IRIS from January 2011 until nowadays





